-
Syphilis remains a significant public health issue in developing countries, with approximately 23%–40% of early untreated or partially treated patients with syphilis presenting with central nervous system involvement, known as neurosyphilis. The manifestations of neurosyphilis are diverse, including dementia, asymptomatic neurosyphilis, meningitis, and meningeal vascular syphilis[1,2]. Meningeal vascular syphilis usually occurs several years after the initial infection and can cause infectious arteritis. This condition leads to stroke-like symptoms that mimic common acute ischemic stroke manifestations. The prevalence of neurosyphilis in patients with stroke ranges from 0.31% to 4.70%[3]. Early treatment of neurosyphilis is crucial for favorable therapeutic outcomes, as delayed treatment can result in irreversible damage[4,5].
Despite the critical need for timely diagnosis, there is no established “gold standard” for diagnosing neurosyphilis. Metagenomic next-generation sequencing (mNGS) technology, while not targeting specific nucleic acids of pathogens, offers broad-spectrum detection and high sensitivity. Its clinical applications are expanding, with research confirming its diagnostic value for infectious diseases of the central nervous system[6,7]. Here, we report a case of neurosyphilis initially diagnosed as a cerebral infarction using cerebrospinal fluid (CSF) mNGS in our hospital.
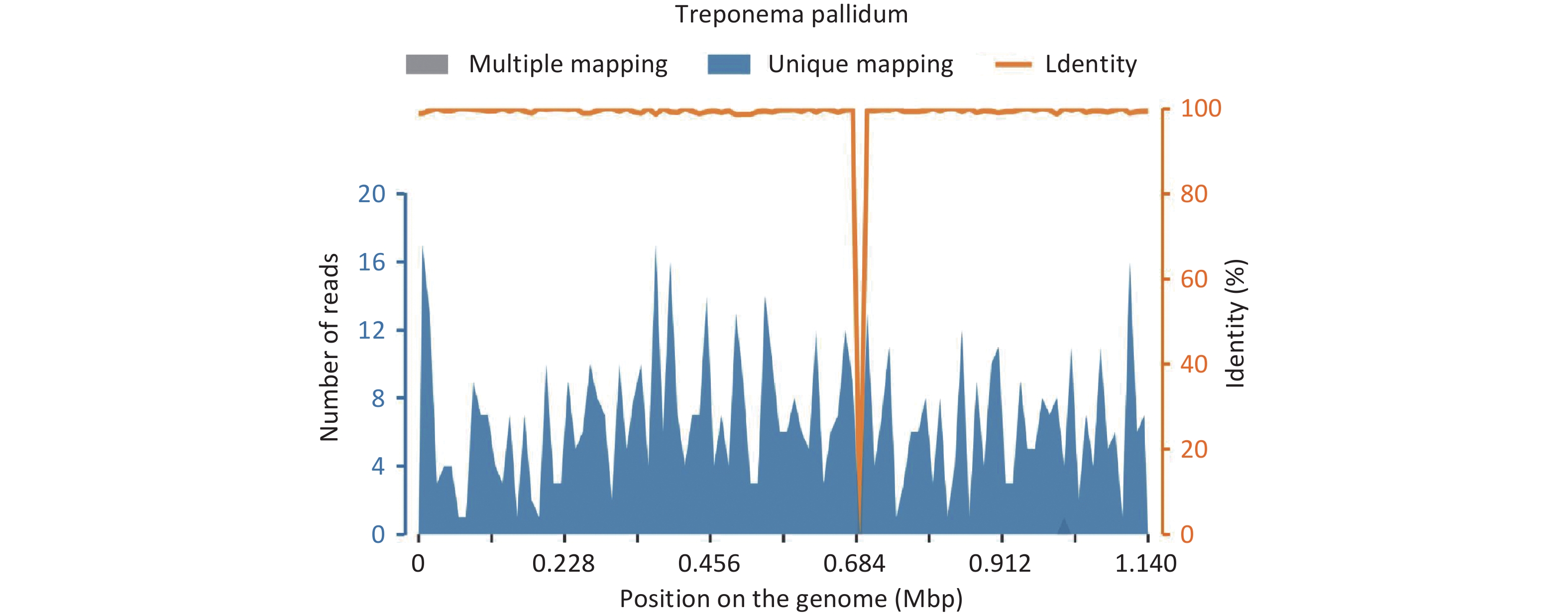
A 59-year-old man was admitted to the Neurology Department of Shanghai East Hospital on August 16, 2023, due to a sudden loss of consciousness and cognitive impairment that lasted for 6 h. The patient denied experiencing dizziness, headache, blurred vision, nausea, vomiting, double vision, or difficulty swallowing. He had a 7-year history of hypertension. Upon examination, the patient was able to follow instructions and complete actions, but could not recognize others, including his wife, and was unaware of his name, identity, age, and address. The neurologic examination revealed that the patient had normal tendon reflexes, a positive finger-nose test, and negative Kernig’s and Brudzinski’s signs. The patient’s blood pressure was measured at 129/67 mmHg. The National Institute of Health Stroke Scale (NIHSS) score was 2, suggesting low stroke-related impairment. The total score of Glasgow Coma Scale (GCS) was 15, indicating that the person is fully awake and oriented. Kubota’s drinking water test showed a level of 1, which is typically considered normal. Serological testing was positive for Treponema pallidum-specific antibodies and for the toluidine red unheated serum test (TRUST) with a titer of 1:32 while the results of serological screening tests for hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) were negative. CSF analysis showed a positive Pandy’s test, an increased white blood cell count (115 × 106/L), and elevated CSF total protein (1,252 mg/L) levels. CSF testing was positive for Treponema pallidum-specific antibodies and for CSF-TRUST with a titer of 1:8. mNGS results confirmed the presence of Treponema pallidum, with 666 sequences and a relative abundance of 7.95%. The coverage map is shown in Figure 1.
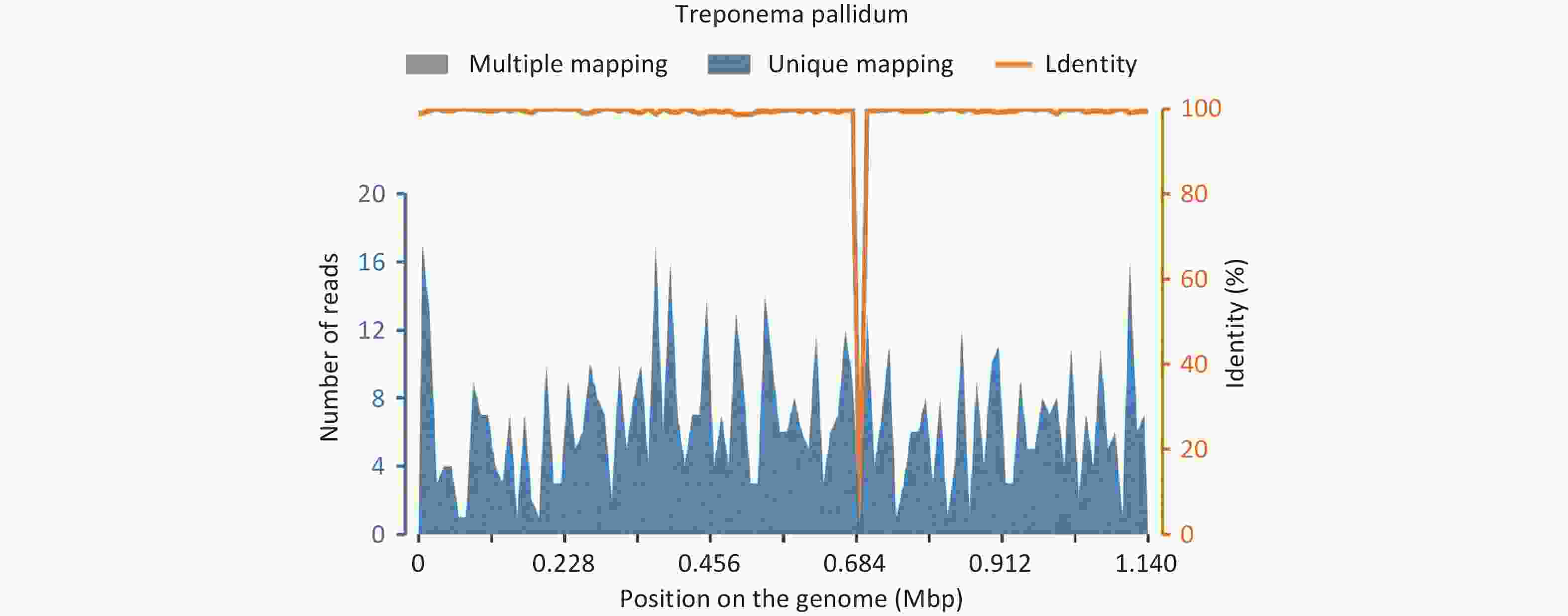
Figure 1. Coverage map of metagenomic next-generation sequencing confirmed Treponema pallidum in the cerebrospinal fluid of the patient.
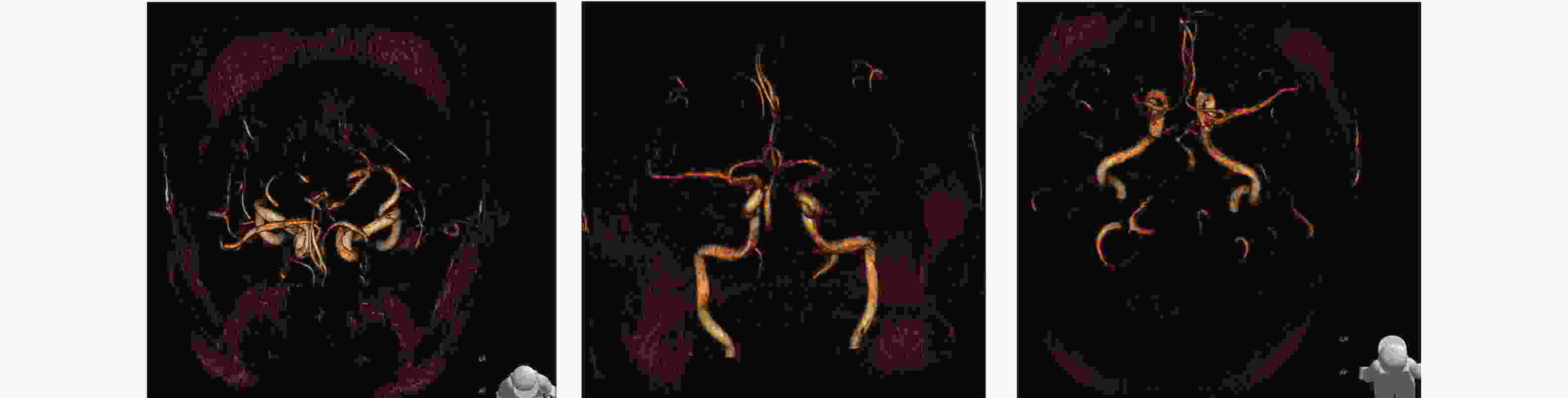
Given the patient’s syphilis infection, we reviewed his medical history. His wife reported that he had been diagnosed with syphilis in 2007 and treated at another hospital with no subsequent follow-up. Magnetic resonance angiography (MRA) revealed the P2 segment and distal segment of the right posterior cerebral artery are not clearly visible, suggesting possible stenosis intracranial arteriosclerosis and a slender right vertebral artery, besides the right vertebral artery is slender, with the V4 segment terminating at the right posterior inferior cerebellar artery (Figure 2).
Brain magnetic resonance imaging (MRI) revealed acute cerebral infarction near the left lateral ventricle using diffusion-weighted imaging (DWI), apparent diffusion coefficient (ADC), T1-weighted imaging (T1WI), T2-weighted imaging (T2WI), and T2 fluid-attenuated inversion recovery (T2FLAIR). Additionally, susceptibility-weighted imaging (SWI) showed hemosiderin deposition in the left parietal lobe. Furthermore, signs of age-related brain and white matter degeneration were noted on the T2FLAIR image (Figure 3).
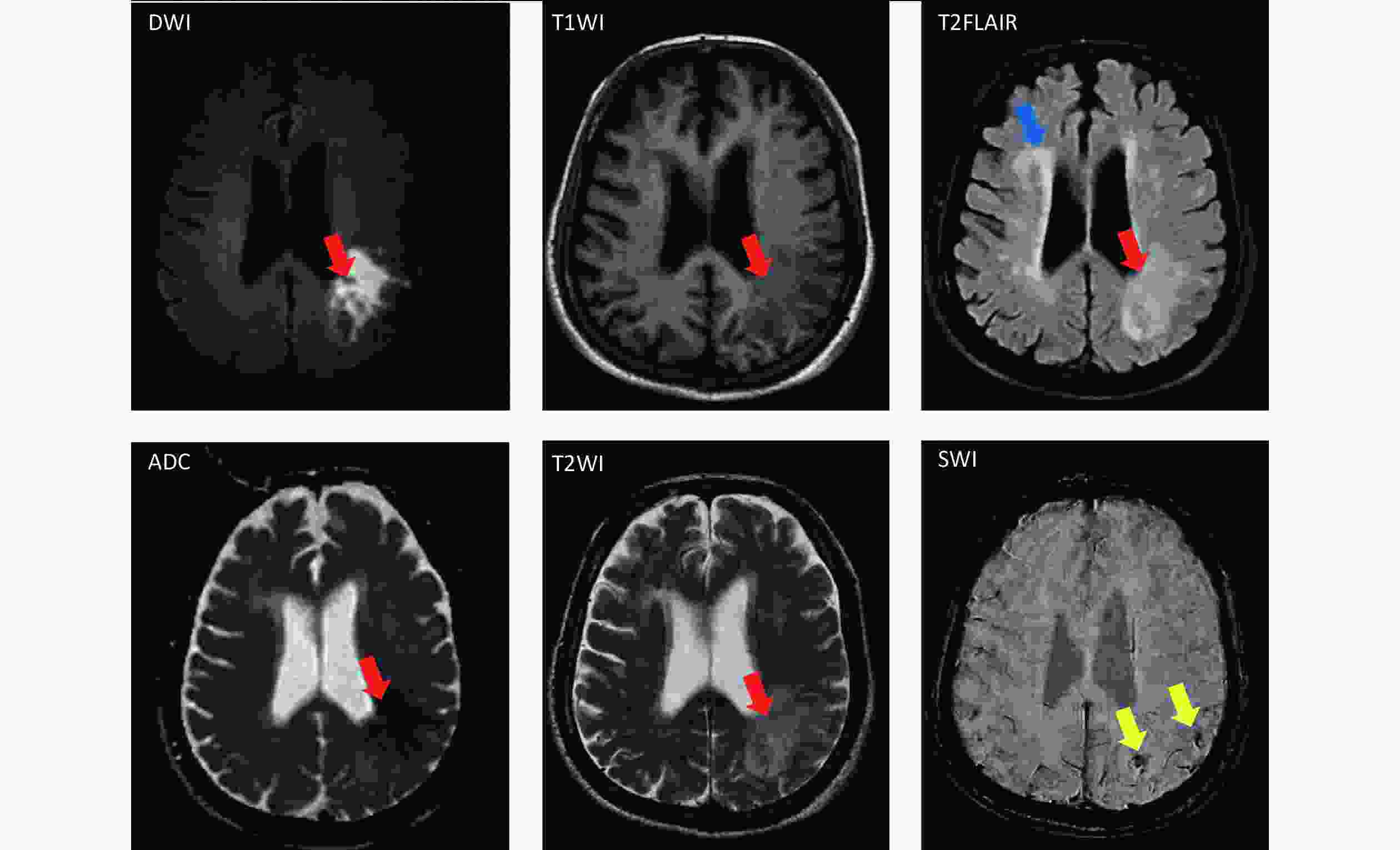
Figure 3. Patient’s brain magnetic resonance imaging scan (red arrow: acute cerebral infarction; blue arrow: brain degeneration and white matter degeneration; and yellow arrow: hemosiderin deposition).
The cranial MRI manifestations in patients with neurosyphilis are diverse but not specific. Most lesions are related to secondary vasculitis, leading to ischemic changes, granulomatous inflammation, and neuronal necrosis[8]. Treponema pallidum can adhere to cell surfaces and the capillary walls through mucopolysaccharides, destroying tissues and blood vessels rich in these substances. This can cause necrosis of the vascular inner and outer membranes and thrombosis, leading to cerebral hypoperfusion in the temporal lobe and limbic system[8]. The patient’s electroencephalogram findings showed sharp waves bilaterally, likely related to neuronal electrophysiological disturbances caused by the syphilis infection.
Based on these results, the patient was diagnosed with cerebral infarction due to syphilitic cerebral arteritis, which caused occlusion of the middle cerebral artery branches. During the acute stage of cerebral infarction, the patient received dual antiplatelet therapy with aspirin and clopidogrel, along with statins to stabilize the plaques. Six million units (6 MU) of penicillin sodium were injected every 6 h for the treatment of neurosyphilis, which led to significant improvement in his mental state after 2 days. Subsequently, he was able to recognize his wife and recall previous work. Remarkably, although penicillin is universally considered as an effective treatment for syphilis, the recommended regimen with benzathine penicillin G (BPG) does not prevent all serological failures and late complications, as neurosyphilis[9]. The occurrence of neurosyphilis in our case was most likely caused by the limitations of the treatment regimen. However, after the patient recovered from neurosyphilis treatment for 2 days, he was transferred to other hospitals with no further information could be traced.
For infectious diseases of the central nervous system, early identification and treatment of the causative pathogens are crucial for improving patient prognosis. The traditional diagnostic model relies on clinical history, manifestations, and imaging results, which often lack specificity for rare pathogens. In addition, the availability and quantity of CSF samples are limited, making traditional methods such as CSF smears and culture challenging for neuroinflammatory diseases[6]. The mNGS technology is more sensitive and less time-consuming than traditional detection methods, and can thus help rapidly identify and diagnose pathogens in clinically difficult cases. However, mNGS technology is complex and can be influenced by many factors, including background microorganisms in the laboratory, reagents, and contamination of skin-colonizing bacteria during lumbar puncture sampling. For cases with high suspicion of tuberculous or cryptococcal meningitis, the host removal process, which reduces human DNA contamination in clinical CSF specimens, is used to improve the sensitivity of mNGS. The host removal process primarily utilizes the properties of saponins to lyse cells, as human cells lack cell walls and are more easily destroyed. This reduces the proportion of human DNA and increases the detection rate of pathogens. However, this process may also lead to the loss of some fragile pathogens, resulting in false negatives[10]. During report interpretation, we integrate the patient’s clinical history, routine CSF test results, etiological findings, and imaging results to ensure the mNGS results align with the clinical context, minimizing false positives. For difficult cases, the laboratory collaborates closely with clinicians and, if necessary, employs advanced technologies such as mass spectrometry and digital PCR for confirmation. In this case, we used routine mNGS procedures on the CSF and detected Treponema pallidum, suggesting that this method can effectively assist in diagnosing neurosyphilis and enhance its diagnostic accuracy. In summary, although mNGS is susceptible to background bacterial contamination, has high costs, can provide false-positive results, it is more effective than traditional detection methods for the diagnosis of central nervous system infections, thereby providing a reliable basis for clinical diagnosis and treatment; further, its use is expected to improve the diagnosis and treatment of central nervous system infectious diseases.
doi: 10.3967/bes2024.167
Diagnostic Value of Cerebrospinal Fluid Sequencing for Neurosyphilis with Cognitive Impairment
-
Abstract: Neurosyphilis (NS) is an infectious disease caused by Treponema pallidum invading the central nervous system. It can manifest at any stage of syphilis, and is often misdiagnosed due to its atypical and progressive symptoms. The increasing incidence of NS underscores the necessity for early and accurate diagnosis. Here, we present a case where routine cerebrospinal fluid metagenomic next-generation sequencing (mNGS) was used to diagnose a patient with neurosyphilis. The patient exhibited cognitive impairment and was initially diagnosed with cerebral infarction due to syphilitic cerebral arteritis. Thus, the patient was treated with dual antiplatelet therapy (aspirin and clopidogrel) and statins to stabilize the plaques. Neurosyphilis was treated with penicillin sodium injections, resulting in significant improvement in the patient’s mental state. This case is a rare instance of neurosyphilis associated with cerebral infarction. These findings suggest that mNGS is a valuable tool in diagnosing neurosyphilis, potentially improving diagnostic accuracy and patient outcomes.
-
Key words:
- Neurosyphilis /
- mNGS /
- Cognitive impairment /
- Cerebral infarction
The authors declare that they have no competing interests.
Written informed consent was obtained from the patient’s family for the publication of this case. No ethical committee approval was required for this study as the data were analyzed in a retrospective manner.
&These authors contributed equally to this work.
注释:1) Authors’ Contributions: 2) Competing Interests: 3) Ethical Approval and Consent to Participate: -
-
[1] Hook III EW. Syphilis. Lancet, 2017; 389, 1550−7. doi: 10.1016/S0140-6736(16)32411-4 [2] Tao YS, Chen MY, Tucker JD, et al. A nationwide spatiotemporal analysis of syphilis over 21 years and implications for prevention and control in China. Clin Infect Dis, 2020; 70, 136−9. doi: 10.1093/cid/ciz331 [3] Targa Martins R, Castilhos RM, Silva da Silva P, et al. Frequency of screening and prevalence of neurosyphilis in stroke population. Cerebrovasc Dis, 2020; 49, 301−6. doi: 10.1159/000508491 [4] Du FZ, Zhang HN, Li JJ, et al. Neurosyphilis in China: a systematic review of cases from 2009-2021. Front Med (Lausanne), 2022; 9, 894841. [5] Gonzalez H, Koralnik IJ, Marra CM. Neurosyphilis. Semin Neurol, 2019; 39, 448−55. doi: 10.1055/s-0039-1688942 [6] Wilson MR, Sample HA, Zorn KC, et al. Clinical metagenomic sequencing for diagnosis of meningitis and encephalitis. N Engl J Med, 2019; 380, 2327−40. doi: 10.1056/NEJMoa1803396 [7] Xing XW, Zhang JT, Ma YB, et al. Metagenomic next-generation sequencing for diagnosis of infectious encephalitis and meningitis: a large, prospective case series of 213 patients. Front Cell Infect Microbiol, 2020; 10, 88. doi: 10.3389/fcimb.2020.00088 [8] Ropper AH. Neurosyphilis. N Engl J Med, 2019; 381, 1358−63. doi: 10.1056/NEJMra1906228 [9] Drago F, Ciccarese G, Broccolo F, et al. A new enhanced antibiotic treatment for early and late syphilis. J Glob Antimicrob Resist, 2016; 5, 64−6. doi: 10.1016/j.jgar.2015.12.006 [10] Ji XC, Zhou LF, Li CY, et al. Reduction of human DNA contamination in clinical cerebrospinal fluid specimens improves the sensitivity of metagenomic next-generation sequencing. J Mol Neurosci, 2020; 70, 659−66. doi: 10.1007/s12031-019-01472-z -




 下载:
下载:



 Quick Links
Quick Links