-
Human brucellosis caused by Brucella spp. is a significant zoonotic disease worldwide and seriously affects human health and husbandry development[1]. Brucella is a facultative intracellular gram-negative coccobacillus and is reproduced in macrophage phagosomes[2]. To date, there were 12 species and 19 biovars in Genus Brucella spp., while Brucella melitensis was the most common species responsivity for the majority of human and animals’ cases, followed by the Brucella abortus and Brucella suis, other species lead to human brucellosis cases occasionally[1,3]. Brucella spp. can pass directly to humans through contact with infected animals or their products, as well as the digestive and respiratory tracts, and fewer cases of infected sexually[4,5]. Brucella spp. often causes chronic debilitating infections in humans and reproductive disorders in livestock and is associated with spontaneous abortions and reduced fecundity[6]. Brucellosis remains a diagnostic dilemma due to misleading and nonspecific manifestations and an increasing trend of unusual presentations[7]. Therefore, human brucellosis is a serious public health concern and affects the livestock breeding industry, socioeconomic, and regional and international animal trade.
Since 1995, human brucellosis has been a reemerging disease in mainland China, and its epidemic pattern has seen significant change over the past decades[8]. The first high peak of the epidemic occurred in 2014, and the affected area expanded from northern pastureland provinces to adjacent grassland and agricultural areas, then to southern coastal and southwestern areas[9]. In 2021, a total of 69,767 cases were reported from 2,083 counties in mainland China, an increase of 47.7% from 2020 (47,425); approximately 95.5% of the total cases were centralized in northern China and 31.8% in Inner Mongolia[10]. The incidence of brucellosis was distinctly seasonal, with a high incidence in spring and summer and an average annual peak in May[11]. During 1999–2008, the annual incidence of the disease varied greatly from 0 to 818.52/100,000 at county levels; the highest incidence of the disease occurred in Abaga county in the center of Inner Mongolia, the spatial distribution of the disease clustered in the northeastern (Hulunbeir) and central (Xilinguole League) districts[12]. Recently, the epidemic situation of human brucellosis in the Xilinguole League was ongoing decreased; however, the incidence is still high compared to other areas of the north[13]. The method of Joinpoint Regression has been used in numerous domains to assess changes in time series data, including things such as cancer mortality rates, motor vehicle collision mortalities, and disease risk[14]. Therefore, this study aimed to explore the trends of epidemic evolution and the spatiotemporal distribution pattern of human brucellosis in the Xilinguole League (Inner Mongolia) to facilitate the design of targeted surveillance and control measures.
-
Reported cases and incidence rate of human brucellosis of the Xilinguole League (Inner Mongolia) were obtained through China’s National Notifiable Disease Reporting System from January 1, 2004, to December 31, 2023. Microsoft Excel 2021 software was used for the data processed and drawn figures, number of reported cases, incidence rate, and average annual growth of annual incidence were applied to characterize the epidemic trends of disease. The average annual growth rate of the annual incidence from 2004 to 2023 was defined as previously reported[9]; the average annual growth rate (%) of the incidence rate was calculated using the power function based on Microsoft Excel 2021 software. The map of the Xilinguole League (Inner Mongolia) is used from the standard map service system (http://bzdt.ch.mnr.gov.cn/), approval number GS (2024) 0650. The study obtained data on human brucellosis cases reported through China’s National Notifiable Disease Reporting System, the study protocol was approved by the ethic committee of national institute of communicable disease control and prevention (grant NO. ICDC-ZM-2024015). All data are anonymous, and had no patients participated in this study, informed consent to participate was not obtained.
-
A joinpoint regression analysis of the incidence of human brucellosis from 2004 to 2023 was performed as previously described[15]. Briefly, the annual percentage change (APC) and the average annual percentage change (AAPC) for each segment were estimated using a joinpoint regression model, with a focus on estimating the temporal trends in the incidence rate of human brucellosis. A maximum of four joint points were set to ensure that the results were credible; P < 0.05 was considered statistically significant different. The Joinpoint Regression Program Version 5.3.0 (Information Management Services Inc., Calverton, MD, USA) from the Statistical Research and Applications Branch of the Surveillance Research Program of the U.S. National Cancer Institute.
-
A retrospective space-time scanning analysis was performed based on the discrete Poisson model by SaTScan v10.1.3, to identify high rates of spatiotemporal clustering of human brucellosis in the Xilinguole League (Inner Mongolia) 2004/1/1 to 2023/12/31. Briefly, the 10% of the studied population was the maximum cluster size, setting the time interval as half a year, the maximum temporal scanning radius was 90 days, and the Monte Carlo simulation was 999 times, based on previously published literature regarding the spatial clustering of brucellosis[16]. The log-likelihood ratio (LLR) of the test statistics was constructed using actual and theoretical cases inside and outside the scanning window. The corresponding scanning window is the aggregation area when the LLR is statistically significant (P < 0.05).
-
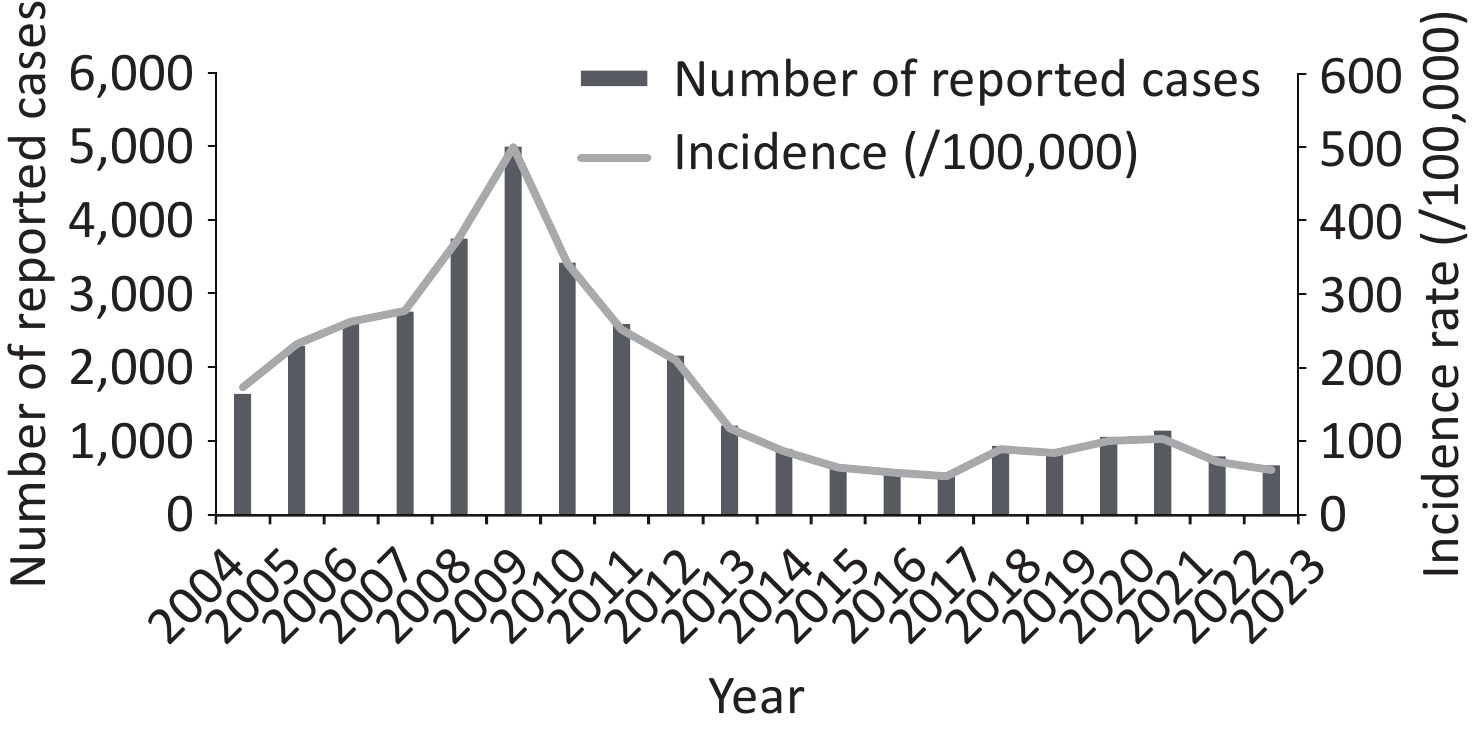
From 2004 to 2023, a total of 35,747 cases were reported, with an annual average of 1787.35 cases and an annual average incidence rate of 176.04/100,000 (Figure 1). Human brucellosis in the Xilinguole League can be divided into two stages: the continuous increase epidemic stage (2004–2009) and the persistent reduction epidemic stage (2010–2023). Since 2004, the incidence rate and number of cases have increased dramatically, peaking in 2009. Following this peak, the incidence persisted and decreased from 2010 to 2017. Subsequently, the reported cases from 2018 started to show slightly higher trends and peaked in 2021; after this, the reported cases continued to reduce. The incidence rate of human brucellosis increased from 173.96/100,000 in 2004 to 500.71/100,000 in 2009 and decreased to 61.43/100,000 in 2023. During the first high epidemic stage, 18,085 cases were reported, with average annual cases and incidence rates of 3,014 and 303.94/100,000, respectively. In the second epidemic period, the average annual number of cases and incidence were 1261.57 and 121.22/100,000, respectively. The fixed base ratio (%) and sequential growth (%) of cases and incidence rate showed that there was a continuous increase trend from 2004 to 2009, then two items decreased after 2010 and had a slight increase from 2020 to 2021 (Table 1).
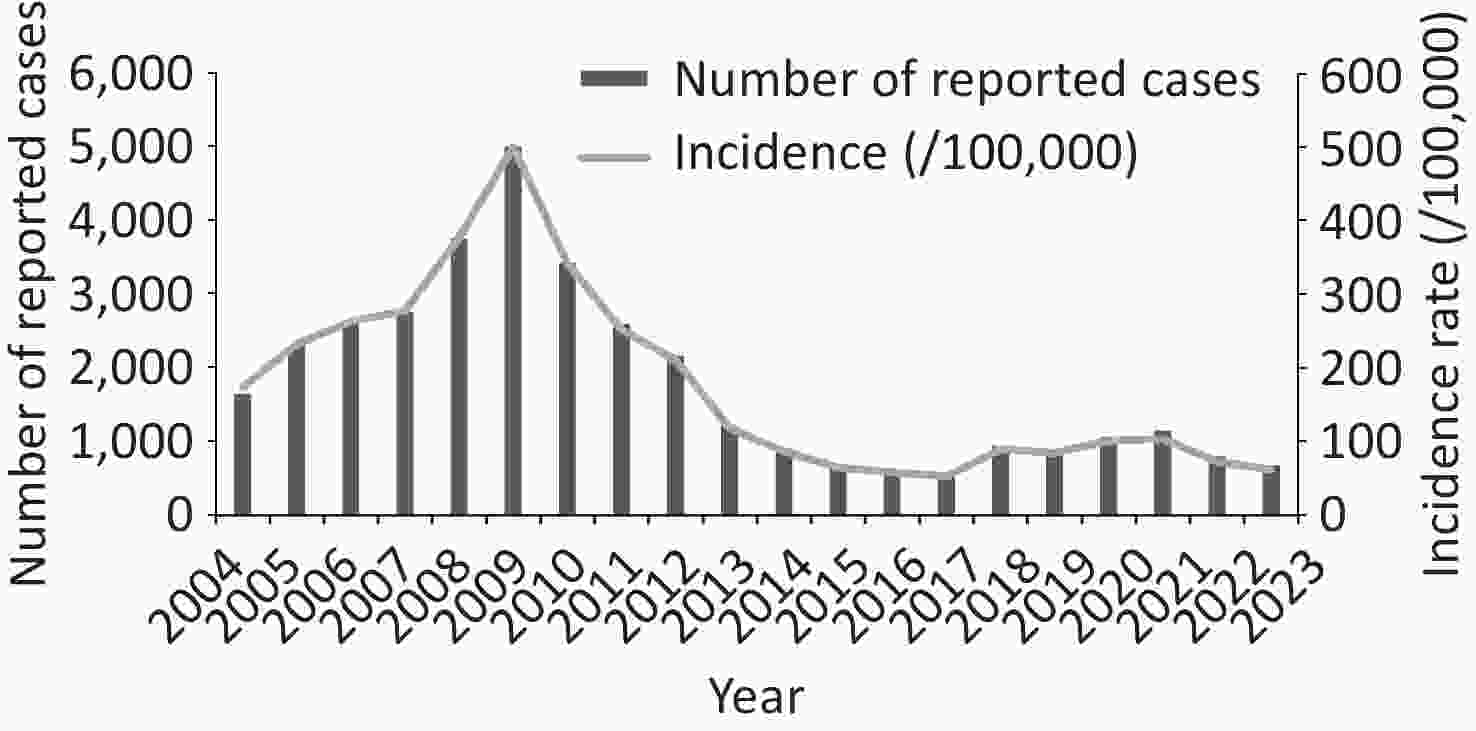
Figure 1. Trends in the epidemic and evolution of human brucellosis in the Xilingol League, from 2004 to 2023. The column chart displayed the total number of reported cases each year, and the curve showed the incidence rate of human brucellosis (/100,000) every year.
Table 1. Epidemic growth trends of cases and incidence from 2004 to 2023
Year Number of cases Incidence (/100,000) Cases Fixed base ratio (%) Sequential growth (%) Incidence Fixed base ratio (%) Sequential growth (%) 2004 1,647 − − 173.96 − − 2005 2,297 0.395 0.395 232.19 0.335 0.335 2006 2,610 0.575 0.136 262.91 0.511 0.132 2007 2,764 0.667 0.059 277.48 0.595 0.055 2008 3,757 1.260 0.359 376.40 1.164 0.356 2009 5,010 2.009 0.334 500.71 1.878 0.330 2010 3,430 1.065 −0.315 342.01 0.966 −0.317 2011 2,597 0.568 −0.243 252.32 0.450 −0.262 2012 2,169 0.312 −0.165 210.37 0.209 −0.166 2013 1,216 −0.257 −0.439 117.82 −0.323 −0.440 2014 899 −0.447 −0.261 86.66 −0.502 −0.265 2015 672 −0.582 −0.253 64.58 −0.629 −0.255 2016 606 −0.622 −0.098 58.12 −0.666 −0.100 2017 553 −0.654 −0.087 52.92 −0.696 −0.090 2018 943 −0.421 0.705 89.67 −0.485 0.694 2019 890 −0.452 −0.056 84.38 −0.515 −0.059 2020 1,067 −0.346 0.199 100.81 −0.420 0.195 2021 1,147 −0.299 0.075 103.61 −0.404 0.028 2022 798 −0.507 −0.304 72.44 −0.584 −0.301 2023 675 −0.581 −0.154 61.43 −0.647 −0.152 Jointpoint regression analysis showed that the epidemic presents a pattern of alternating rise and fall, dramatic increase from 2004 to 2009 (APC = 21.73, P > 0.001), then rapid decrease from 2009 to 2016 (APC= –27.34, P > 0.001), and re-increased slightly from 2016 to 2020, APC = 21.51, P > 0.001) to decreased again from 2020 to 2023 (APC = –21.06, P > 0.001) (Figure 2 and Table 2). These data showed that human brucellosis has decreased significantly. However, the epidemic situation is still severe and has a high risk of rebound, so it is urgent to implement a strict and persistent surveillance program.
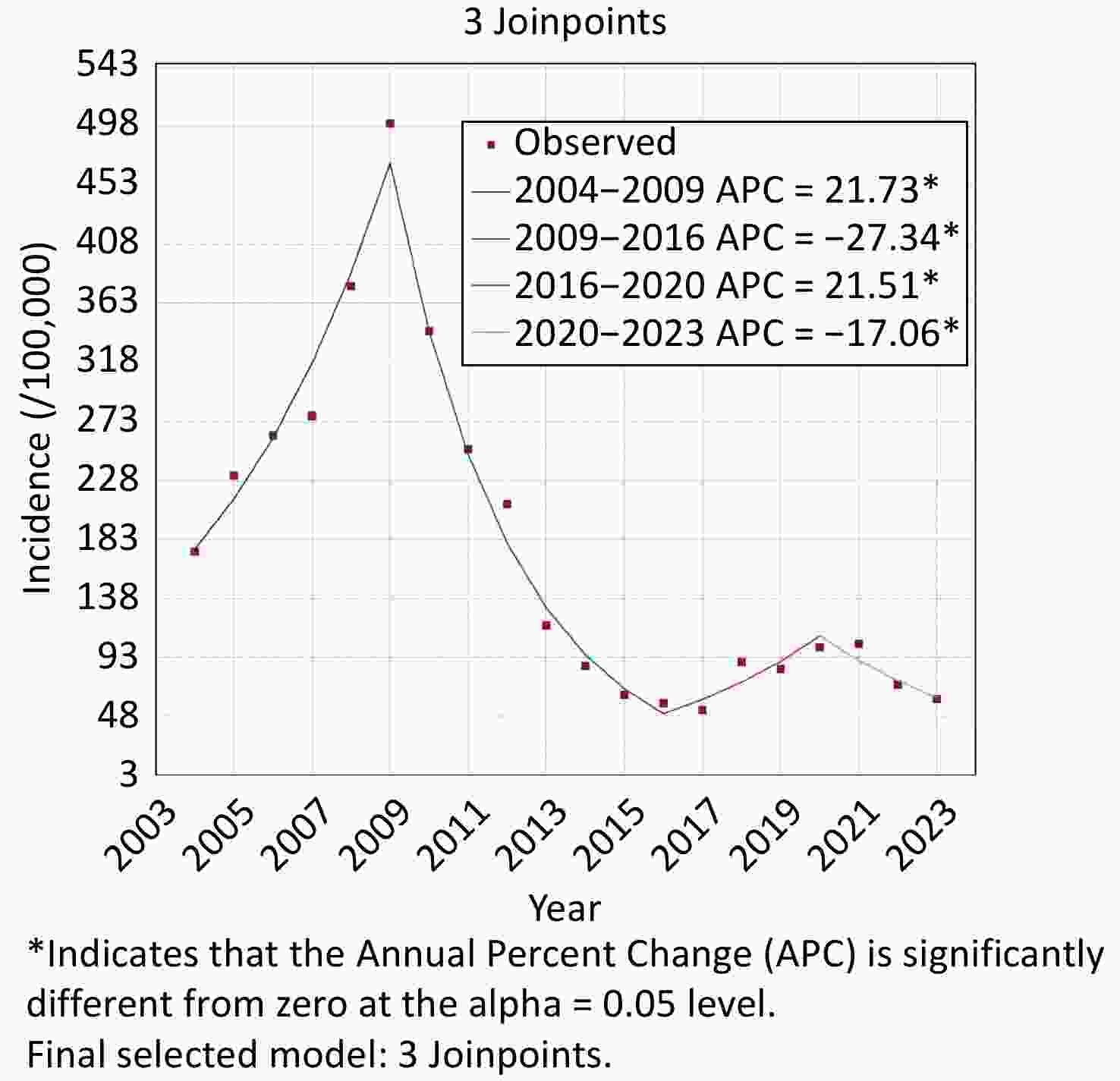
Figure 2. Joinpoint regression analysis of human brucellosis in the Xilingol League in Inner Mongolia from 2004 to 2023. Color indicates the different changes in epidemic trends, *: refers to a significant change trend (P < 0.05).
Table 2. The APC, AAPC, and P-value in joint point regression analysis in this study
Joint point Segment Segment Start Segment End APC/AAPC 95% LCL 95% UCL P−Value APC 0 2004 2009 21.7285 11.4227 31.4655 0.002 1 2009 2016 −27.3421 −32.5713 −23.627 0.002 2 2016 2020 21.5097 10.545 45.2007 0.008 3 2020 2023 −17.0627 −32.374 −6.4092 0.008 AAPC 0 2004 2023 −5.3002 −7.2752 −3.798 0.001 -
Cases were reported in all 13 counties (Banner), the range of numbers of reported cases in different counties (Banner) was ranged from 226 to 4,777 (Table 3 and Figure 3). Based on the reported cases, the most cases of human brucellosis were reported in Xilinhot City (n = 4,777), followed by 4,391 in Sonid Left Banner, 4,324 in Abaga Banner, 3,392 in Zhenglan Banner, 2,958 in East Ujimqin County, 2,897 in West Ujimqin County, 2,800 in Zhengxiangbai Banner, 2,570 in Duolun county, 2,442 in Sonid right Banner, 2,322 in Boarder Yellow Banner, 2,232 in Taibus Banner, 402 in Wulagai Management District, and 226 in Erenhot City (Table 3 and Figure 3). Based on the incidence rate, the range of average annual incidence was from 21.14/100,00 to 585.21/100,000, the highest average annual incidence recorded in Sonid Left Banner (585.21/100,000), 470.01/100,000 in Abaga Banner, 406.93/100,000 in Boarder Yellow Banner, 238.96/100,000 in Zhengxiangbai Banner, 222.40/100,000 in Zhenglan Banner, 175.50/100,000 in East Ujimqin County, 175.00/100,000 in West Ujimqin County, 165.28/100,000 in Sonid Right Banner, 119.56/100,000 in Xilinhot City, 119.29/100,000 in Duolun County, 85.48/100,000 in Taibus Banner, 80.42/100,000 in Wulagai Management District, and 21.14/100,000 in Erenhot City (Table 3 and Figure 3). Meanwhile, the range of the average annual growth rate of the incidence was from –0.137 (Abaga Banner) to 0.053 (Erenhot City); these data imply that the incidence rate continuously decreased in all counties, but the incidence rate is still high (Table 3).
Table 3. The reported cases, incidence, and average annual growth rate (%) on county levels
Counties Numbers of reported cases Average annual
incidence (/100,000)Average annual growth rate (%) Abaga Banner 4,324 470.01 −0.137 Boarder Yellow Banner 2,322 406.93 −0.111 Xilinhot City 4,777 119.56 −0.077 Duolun county 2,570 119.29 −0.073 Wulagai Management District 402 80.42 −0.068 Sonid Left Banner 4,391 585.21 −0.064 Sonid right Banner 2,442 165.28 −0.057 Taibus Banner 2,232 85.48 −0.005 Zhenglan Banner 3,392 222.40 0.009 East Ujimqin County 2,958 175.50 0.018 West Ujimqin County 2,897 175.00 0.026 Zhengxiangbai Banner 2,800 238.96 0.043 Erenhot City 226 21.14 0.053 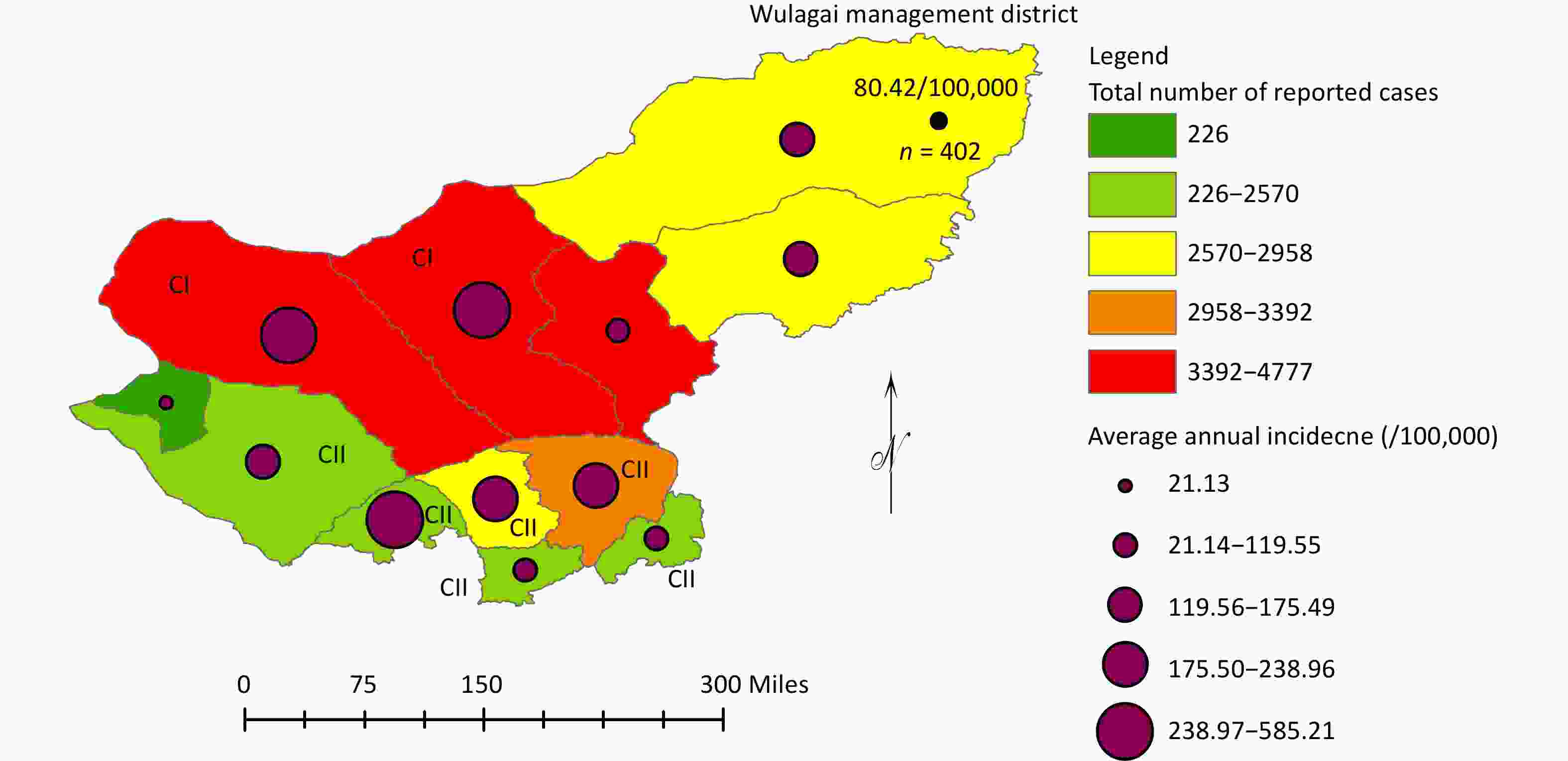
Figure 3. Geographic distribution pattern of the number of cases reported and the average annual incidence rate (/100,000) of human brucellosis in the Xilingol League. Color is used to mark the number of reported cases in different counties, and the purple circle size indicates the range of average annual incidence rate at the county level; the black dot indicates the total number of reported cases (n = 402), and the average annual incidence rate (80.42/100,000) in Wulagai management district; and CI and CII in this figure indicates that location of counties in two high clusters. Map approved number: GS (2024) 0650.
-
Spatiotemporal analysis revealed that two high clusters (CⅠ and CⅡ) were found in 2023; two clusters were concentrated in areas of the west that comprised eight counties (Figure 4). The first high cluster consisted of two counties and the period spanned from January 2005 to December 2011, with a scanning radius of 107.02 km, characterized by a high LLR of 7118.97, an RR of 7.5, and P < 0.001 (Figure 4). The second high cluster comprised six counties, with a scanning radius of 236.40 km and a time frame extended from January 2008 to December 2012, with an LLR of 1125. 01, an RR of 1.93, and a P < 0.001 (Figure 4). These data highlight that the high clusters of the north shifted to the south parts, the Xilinguole League, and the high incidence rate was mainly concentrated from 2005 to 2012; after this, the incidence gradually decreased.
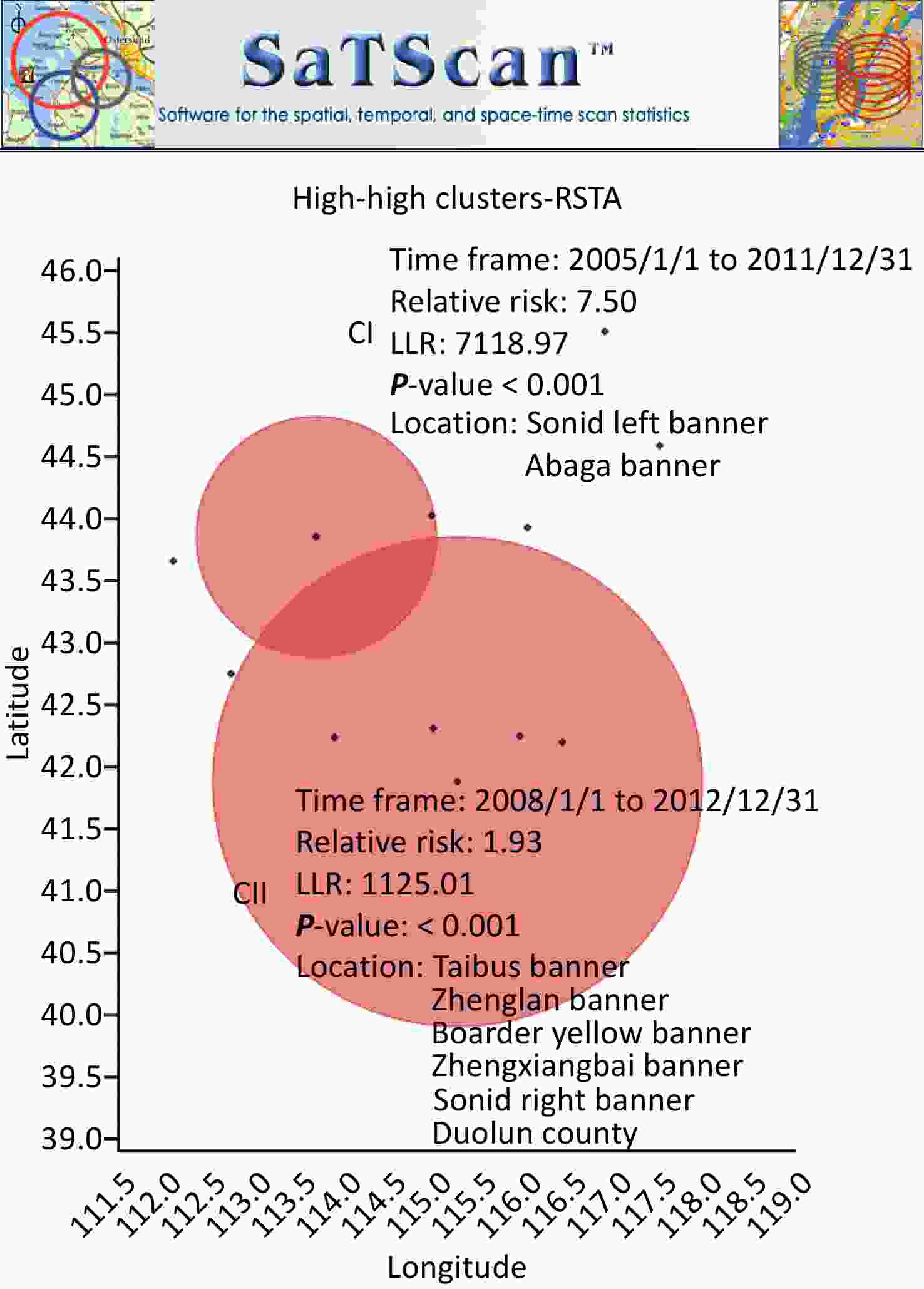
Figure 4. Temporal-spatial cluster characteristics of human brucellosis in the Xilingol League from 2004 to 2023. The figure shows a retrospective space-time analysis scanning for clusters with high rates using the discrete Poisson model; the red circle size indicates the coordinates and radius of high-risk clusters; the X-axis is longitude, the Y-axis is latitude; and the cluster time frame, relative risk, LLR, and P-value of two high clusters are also marked.
-
Human brucellosis was an epidemic disease in the Xilinguole League, and suspected cases of human brucellosis were reported in the Boarder Yellow Banner and Zhengxiangbai Banner in 1922[17]. In 1952, two human cases and 44 infected sheep were detected on the Xilingol League livestock farm based on the serum tube agglutination test[17], these data showed that brucellosis is an epidemic disease in the Xilingol League. During the epidemic peak of brucellosis in this region in 1950−1960s, 544 cases were reported[18]. Subsequently, a comprehensive control measure including S2 vaccine (Brucella suis) drinking immunization in livestock[19], quarantine, and elimination of infected livestock were implemented in the 1970s and 1980s; the disease has been effectively controlled, and only 53 cases were reported from 1970 to 1990, and the incidence rate in four counties was less than 1.00/100,000, and another four counties had no cases reported for five consecutive years[18,20].
Since the 1990s, human brucellosis has become a re-merging disease, and incidence has continuously increased since 2000[9]. In 2002, the seropositive rate was 5.67%, 402 new cases were found nationwide based on the serum surveillance of 12 national key monitor points of human brucellosis, 78.61% new cases were detected in Xilingol League, Inner Mongolia, there were seven human and livestock outbreak events recorded, and 16 Brucella strains were isolated from animals’ samples, and 14 strains were identified as B. melitensis, and the remaining two strains were B. suis[21]. These data imply that brucellosis has been re-emerging in Xilingol League; the incidence rate increased from 173.96/100,000 in 2004 to 500.71/100,000 in 2009 and then fluctuated decreased to 61.43/100,000 in 2023. Xilingol League is pastoral areas, livestock free range is the most common feeding type, introduce breeding and cross areas trade and transfer of livestock was frequent, herdsmen conceal the feeding, introduction, and abortion situation, these factors were co-driven the human brucellosis persistent circulating and spread in this region[22]. The epidemic peak presented in this study occurred in 2009; it was earlier than the epidemic peak in Inner Mongolia (2011) and Notional (2014). In Inner Mongolia, the first epidemic peak of human brucellosis was reported in 2011, a total of 17,320 cases were reported, with an incidence of 70.10/100,000[23]. In China, human brucellosis was at a historical high that occurred in 2014, and the incidence was 4.2 cases/per 100,000 residents in 2014[9]. Therefore, further pathogen surveillance and genomic epidemiological investigations will provide information to better understand the detailed role of the Xilingol League in the brucellosis epidemic in Inner Mongolia and nationwide.
Human brucellosis was continuously decreased in the Xilingol League due to the exercise of a set of surveillance and control measures. Since 2007, the government has taken various measures to promote and educate high-risk populations for brucellosis, as well as conduct behavioral interventions to improve their knowledge of brucellosis prevention and control, change unhealthy habits, and achieve the effect of preventing brucellosis[18]. Since 2008, Inner Mongolia has implemented comprehensive prevention and control measures such as mandatory immunization of cattle and sheep brucellosis vaccines and cow health surveys throughout the region, and later launched inter-animal tracing and eradication work, including all susceptible livestock are vaccinated with live vaccine before mating, and the immunization density reaches 100%, and infect animal serum screen work is also carried out, the outbreak of brucellosis in livestock has been preliminarily controlled, leading to a significant decrease in the level of brucellosis in humans[24]. The epidemic in mid-eastern Inner Mongolia has decreased; however, the epidemic has worsened in western Inner Mongolia[13]. In Hulun Buir City, Inner Mongolia, a total of 23,897 cases of human brucellosis were reported between 2003 and 2018, with an incidence rate of 56.03/100,000, which is 20 times higher than the average incidence of the country[25]. In Hulun Buir City, the incidence rates in developed areas of animal husbandry (Horqin Youyi Qianqi and Horqin Youyi Zhongqi) were significantly higher than in forest areas (Arxan)[26]. The areas of central and eastern Inner Mongolia provide a suitable long-term environment, where human brucellosis outbreaks have occurred and it can be expected that they will persist[27]. Disease control in these regions was extremely difficult because livestock farming is the only source of income, a nomadic lifestyle, and low socioeconomic levels[28]. In this study, the epidemic situation of different counties has significant differences; the distribution pattern of disease was related closely to the local industry construct, and the least cases were recorded in Erenhot City, which is a trade port city between Mongolia and China. A recent study has identified high-risk areas and the driving effect of brucellosis along the borders between China and Mongolia. Furthermore, there is the possibility of cross-border wildlife activities in high-risk areas, increasing the risk of cross-border brucellosis transmission[29]. Therefore, continuous investment and surveillance are a priority in regions with high incidence, and especially massive ruminate immunization plans are necessary against animal brucellosis to reduce human population infection. Furthermore, the Xilingol League is adjacent to many regions where brucellosis is rampant and greater oversight of animal transfer and illegal trade is urged.
In this study, a landscape map of epidemic evolution trends and spatiotemporal clustering of human brucellosis in Xilingol League, Inner Mongolia, over two decades were constructed. Although human brucellosis showed a significantly decreased trend, incidences remain higher than in other regions; further strengthening of surveillance and control is recommended. Furthermore, our study also identified the large clusters of human brucellosis. These data will provide vital clues for the public health department in devising, developing, and exerting effective targeted control measures and allocation of medicine resources. In the next step, we need to implement pathogen surveillance and genomic epidemiology to provide more comprehensive information to understand the transmission pattern and transmission dynamic.
doi: 10.3967/bes2025.081
Epidemic Evolution Trends and Spatiotemporal Clustering of Human Brucellosis in Xilingol League Inner Mongolia, from 2004 to 2023
-
Abstract:
Objective Human brucellosis is a serious public health concern in the Xilingol League, Inner Mongolia; however, the epidemic trends are unclear. Method In this study, Joinpoint regression analysis and spatiotemporal analysis were applied to investigate the epidemic evolution of human brucellosis. Result From 2004 to 2023, a total of 35,747 cases were reported, with an annual average of 1787.35 cases and an annual average incidence rate of 176.04/100,000. The incidence increased from 173.96/100,000 in 2004 to 500.71/100,000 in 2009 and fluctuated to 61.43/100,000 in 2023. Three epidemic join points were observed in which the disease experienced an alternative rise and fall, peaking in 2009 (APC = 21.73, P > 0.001) and 2020 (APC = 21.51, P > 0.001). The disease showed a persistent decline trend in lentitude (AAPC = –5.30, P > 0.001), suggesting challenges in disease control and a higher risk of rebound. The most cases were reported in Xilinhot City (n = 4,777), followed by 4,391 in Sonid Left Banner, and 4,324 in Abaga Banner. Spatiotemporal analysis revealed two high clusters (CⅠ and CⅡ) from 2005 to 2012, the high cluster encompassing eight counties and shifting from north to south. Conclusion The present analysis highlights that human brucellosis has decreased significantly in the Xilingol League, but the epidemic is still severe; further implementation of a strict control program is necessary. -
Key words:
- Human brucellosis /
- Epidemiological /
- Joinpoint regression analysis /
- Spatiotemporal analysis
The authors have no conflicts of interest to declare.
&These authors contributed equally to this work.
注释:1) Authors’ Contributions: 2) Competing Interests: -
Figure 3. Geographic distribution pattern of the number of cases reported and the average annual incidence rate (/100,000) of human brucellosis in the Xilingol League. Color is used to mark the number of reported cases in different counties, and the purple circle size indicates the range of average annual incidence rate at the county level; the black dot indicates the total number of reported cases (n = 402), and the average annual incidence rate (80.42/100,000) in Wulagai management district; and CI and CII in this figure indicates that location of counties in two high clusters. Map approved number: GS (2024) 0650.
Figure 4. Temporal-spatial cluster characteristics of human brucellosis in the Xilingol League from 2004 to 2023. The figure shows a retrospective space-time analysis scanning for clusters with high rates using the discrete Poisson model; the red circle size indicates the coordinates and radius of high-risk clusters; the X-axis is longitude, the Y-axis is latitude; and the cluster time frame, relative risk, LLR, and P-value of two high clusters are also marked.
Table 1. Epidemic growth trends of cases and incidence from 2004 to 2023
Year Number of cases Incidence (/100,000) Cases Fixed base ratio (%) Sequential growth (%) Incidence Fixed base ratio (%) Sequential growth (%) 2004 1,647 − − 173.96 − − 2005 2,297 0.395 0.395 232.19 0.335 0.335 2006 2,610 0.575 0.136 262.91 0.511 0.132 2007 2,764 0.667 0.059 277.48 0.595 0.055 2008 3,757 1.260 0.359 376.40 1.164 0.356 2009 5,010 2.009 0.334 500.71 1.878 0.330 2010 3,430 1.065 −0.315 342.01 0.966 −0.317 2011 2,597 0.568 −0.243 252.32 0.450 −0.262 2012 2,169 0.312 −0.165 210.37 0.209 −0.166 2013 1,216 −0.257 −0.439 117.82 −0.323 −0.440 2014 899 −0.447 −0.261 86.66 −0.502 −0.265 2015 672 −0.582 −0.253 64.58 −0.629 −0.255 2016 606 −0.622 −0.098 58.12 −0.666 −0.100 2017 553 −0.654 −0.087 52.92 −0.696 −0.090 2018 943 −0.421 0.705 89.67 −0.485 0.694 2019 890 −0.452 −0.056 84.38 −0.515 −0.059 2020 1,067 −0.346 0.199 100.81 −0.420 0.195 2021 1,147 −0.299 0.075 103.61 −0.404 0.028 2022 798 −0.507 −0.304 72.44 −0.584 −0.301 2023 675 −0.581 −0.154 61.43 −0.647 −0.152 Table 2. The APC, AAPC, and P-value in joint point regression analysis in this study
Joint point Segment Segment Start Segment End APC/AAPC 95% LCL 95% UCL P−Value APC 0 2004 2009 21.7285 11.4227 31.4655 0.002 1 2009 2016 −27.3421 −32.5713 −23.627 0.002 2 2016 2020 21.5097 10.545 45.2007 0.008 3 2020 2023 −17.0627 −32.374 −6.4092 0.008 AAPC 0 2004 2023 −5.3002 −7.2752 −3.798 0.001 Table 3. The reported cases, incidence, and average annual growth rate (%) on county levels
Counties Numbers of reported cases Average annual
incidence (/100,000)Average annual growth rate (%) Abaga Banner 4,324 470.01 −0.137 Boarder Yellow Banner 2,322 406.93 −0.111 Xilinhot City 4,777 119.56 −0.077 Duolun county 2,570 119.29 −0.073 Wulagai Management District 402 80.42 −0.068 Sonid Left Banner 4,391 585.21 −0.064 Sonid right Banner 2,442 165.28 −0.057 Taibus Banner 2,232 85.48 −0.005 Zhenglan Banner 3,392 222.40 0.009 East Ujimqin County 2,958 175.50 0.018 West Ujimqin County 2,897 175.00 0.026 Zhengxiangbai Banner 2,800 238.96 0.043 Erenhot City 226 21.14 0.053 -
[1] Whatmore AM, Foster JT. Emerging diversity and ongoing expansion of the genus Brucella. Infect Genet Evol, 2021; 92, 104865. doi: 10.1016/j.meegid.2021.104865 [2] Iranikhah M, Nazari R, Fasihi-Ramandi M, et al. Immunogenicity of Brucella trivalent immunogen-containing polyethyleneimine nanostructure targeted with LPS in a mouse model. Curr Microbiol, 2024; 81, 383. doi: 10.1007/s00284-024-03824-4 [3] Attia El Hili H, Maatouk K. Zoonotic potential of brucellosis in marine mammals. Med Trop Sante Int, 2024; 4, mtsi. v4i1.2024. 489. [4] Liu BF, Liu GT, Ma XP, et al. Epidemiology, clinical manifestations, and laboratory findings of 1, 590 human brucellosis cases in Ningxia, China. Front Microbiol, 2023; 14, 1259479. doi: 10.3389/fmicb.2023.1259479 [5] Li NN, Yu F, Peng FY, et al. Probable sexual transmission of brucellosis. IDCases, 2020; 21, e00871. doi: 10.1016/j.idcr.2020.e00871 [6] La THA, McMillan IA, Dahal P, et al. Tracking sero-molecular trends of swine brucellosis in Hawai'i and the central Pacific. Front Public Health, 2024; 12, 1440933. doi: 10.3389/fpubh.2024.1440933 [7] Anadure RK, Goel J, Sahu S, et al. Recurrent encephalopathy with transverse myelitis: an uncommon presentation of neurobrucellosis. J Neurosci Rural Pract, 2019; 10, 703−6. doi: 10.1055/s-0039-1700600 [8] Shang DQ, Xiao DL, Yin JM. Epidemiology and control of brucellosis in China. Vet Microbiol, 2002; 90, 165−82. doi: 10.1016/S0378-1135(02)00252-3 [9] Lai SJ, Zhou H, Xiong WY, et al. Changing epidemiology of human brucellosis, China, 1955-2014. Emerg Infect Dis, 2017; 23, 184−94. doi: 10.3201/eid2302.151710 [10] Yang HM, Chen QL, Li Y, et al. Vital surveillances: epidemic characteristics, high-risk areas and space-time clusters of human brucellosis — China, 2020–2021. China CDC Wkly, 2023; 5, 17−22. doi: 10.46234/ccdcw2023.004 [11] Chen H, Lin MX, Wang LP, et al. Driving role of climatic and socioenvironmental factors on human brucellosis in China: machine-learning-based predictive analyses. Infect Dis Poverty, 2023; 12, 36. doi: 10.1186/s40249-023-01087-y [12] Zhang WY, Guo WD, Sun SH, et al. Human brucellosis, Inner Mongolia, China. Emerg Infect Dis, 2010; 16, 2001−3. doi: 10.3201/eid1612.091081 [13] Cao N, Guo SY, Yan T, et al. Epidemiological survey of human brucellosis in Inner Mongolia, China, 2010-2014: a high risk groups-based survey. J Infect Public Health, 2018; 11, 24−9. doi: 10.1016/j.jiph.2017.02.013 [14] Gillis D, Edwards BPM. The utility of joinpoint regression for estimating population parameters given changes in population structure. Heliyon, 2019; 5, e02515. doi: 10.1016/j.heliyon.2019.e02515 [15] Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med, 2000; 19, 335−51. doi: 10.1002/(SICI)1097-0258(20000215)19:3<335::AID-SIM336>3.0.CO;2-Z [16] Zhang N, Fang XY, Zhou WZ, et al. Epidemiological characteristics and temporal-spatial clustering analysis on human brucellosis in Jiangsu Province, 2006-2021. Sci Rep, 2023; 13, 20024. doi: 10.1038/s41598-023-46690-z [17] Wang DL, Li Y, Li TF, et al. Exploration of new methods for the prevention and control of brucellosis in China. People’s Medical Publishing House. 2018. (In Chinese) [18] Liu MQ, Ge RL, Bi YW. Epidemic analysis on human brucellosis in Xilin Gol League. Chin J Ctrl Endem Dis, 2013; 28, 364−5. (In Chinese) [19] Zhu LQ, Feng Y, Zhang G, et al. Brucella suis strain 2 vaccine is safe and protective against heterologous Brucella spp. infections. Vaccine, 2016; 34, 395−400. doi: 10.1016/j.vaccine.2015.09.116 [20] Chen WJ, Cui BY, Zhang QH, et al. Analysis of epidemic characteristics on brucellosis in Inner Mongolia. Chin J Ctrl Endem Dis, 2008; 23, 56−8. (In Chinese) [21] Zhao YL, Wang DL, Gang SL. Analysis of monitor results of national major monitoring point for brucellosis in 2002. Chin J Ctrl Endem Dis, 2003; 18, 297−8. (In Chinese) [22] Bao H, Bai BX, Mu L. Risk assessment of tracing and investigation of brucellosis in Xilingol League. Vet Orientat, 2018; 49-50. (In Chinese) [23] Liu SJ, Soontornchai S, Bovornkitti S, et al. Epidemiological characteristics and spatio-temporal clusters of human brucellosis in Inner Mongolia, 2010-2021. BMC Infect Dis, 2024; 24, 1321. doi: 10.1186/s12879-024-10165-x [24] Yang Y, Wu G. A brief analysis on prevention and control strategies for brucellosis. World's Latest Medical Information Digest (Electronic Version). 2015. [25] Liu ZG, Liu DY, Wang M, et al. Human brucellosis epidemiology in the pastoral area of Hulun Buir city, Inner Mongolia autonomous region, China, between 2003 and 2018. Transbound Emerg Dis, 2022; 69, 1155−65. doi: 10.1111/tbed.14075 [26] Yuan HT, Wang CL, Liu LN, et al. Epidemiologically characteristics of human brucellosis and antimicrobial susceptibility pattern of Brucella melitensis in Hinggan League of the Inner Mongolia Autonomous Region, China. Infect Dis Poverty, 2020; 9, 79. doi: 10.1186/s40249-020-00697-0 [27] Jia P, Joyner A. Human brucellosis occurrences in Inner Mongolia, China: a spatio-temporal distribution and ecological niche modeling approach. BMC Infect Dis, 2015; 15, 36. doi: 10.1186/s12879-015-0763-9 [28] Liu ZG, Gao LP, Wang M, et al. Long ignored but making a comeback: a worldwide epidemiological evolution of human brucellosis. Emerg Microbes Infect, 2024; 13, 2290839. doi: 10.1080/22221751.2023.2290839 [29] Gao S, Peng RH, Zeng Z, et al. Risk transboundary transmission areas and driving factors of brucellosis along the borders between China and Mongolia. Travel Med Infect Dis, 2023; 56, 102648. doi: 10.1016/j.tmaid.2023.102648 -




 下载:
下载:



 Quick Links
Quick Links