-
Globally, cardiovascular disease (CVD) remains the leading cause of mortality, with the 2023 World Heart Report identifying ischemic heart disease (IHD) as the major contributor to CVD deaths. In 2022, the global age-standardized disability-adjusted life years for IHD is the highest among all diseases, at 2,275.9 per 100,000 people[1]. Therefore, understanding and managing IHD risk factors is critical for disease prevention and health promotion. While well-established risk factors, such as obesity, unhealthy behaviors, and metabolic disorders, are widely recognized, increasing attention has been given in recent years to poor social health as a modifiable risk factor[2].
Poor social health is commonly categorized into two constructs: loneliness and social isolation (SI), each of which affects health differently and independently. Loneliness is defined as the subjective feeling of unpleasantness due to a lack of connection with others[3], while SI refers to the objective lack of relationships and infrequent social contact with family, friends, or the community[4]. Given their distinct characteristics, it is essential to distinguish between these two concepts and examine their independent associations with IHD.
In 2016, a systematic review was the first to suggest that loneliness and SI together increase the risk of IHD by 29%[5]. Since then, observational studies have investigated the impact of poor social health on IHD, but results remain inconsistent due to the influence of confounders, such as conventional biological, behavioral, socioeconomic, and psychological risk factors[6-8]. For instance, a cohort study of 57,825 community-dwelling women in the United States found that higher levels of loneliness and SI were associated with an 8.0% and 5.0% higher risk of incident CVD, respectively[6]. In contrast, a study of 479,054 individuals from the UK Biobank (UKB) database observed no significant association between loneliness, SI, and acute myocardial infarction (MI) after adjusting for possible confounders[7]. These discrepancies may be explained by potential confounders and reverse causality in observational studies. Additionally, patients with CVD have reported feelings of loneliness or SI[9].
Therefore, although some researches have explored the link between poor social health and IHD, it remains unclear whether bidirectional causality exists. Another important question is the potential mediating pathways. Epidemiological studies have associated poor social health with several lifestyle, metabolic, and mental health factors, all of which are modifiable and may influence subsequent IHD risk[10-12]. However, the extent to which these risk factors mediate the relationship requires further investigation.
A Mendelian randomization (MR) study is a causal inference approach that uses single nucleotide polymorphisms (SNPs), which are fixed at conception and naturally randomly assigned to individuals, as instrumental variables[13]. This design minimizes confounding bias and reverse causality often encountered in observational studies[13]. A network MR study is an extended approach that investigates potential mediation effects in causal pathway, addressing the bias issues present arising from confounders and measurement errors in traditional non-instrumental variable methods[14].
In this study, we conducted a bidirectional MR analysis to evaluate the causal relationship between poor social health and IHD using available genome-wide association studies (GWAS) summary-level data from the UKB cohort and the CARDIoGRAMplusC4D Consortium. Furthermore, we applied network MR analyses to assess whether 20 candidate mediators, including metabolic, behavioral, and psychological factors, play a mediating role in the causal pathway from poor social health to IHD. These analyses provide causal evidence for the role of poor social health in the development of IHD, helping to enhance our understanding of IHD’s underlying causes and inform prevention strategies to curb its prevalence.
-
An overview of the study design is shown in Figure 1. This study is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology Using MR guidelines[15]. Ethical approval and consent were obtained in the original GWASs. This study used only summary-level data from relevant GWASs; thus, no additional ethical approval or informed consent was required.
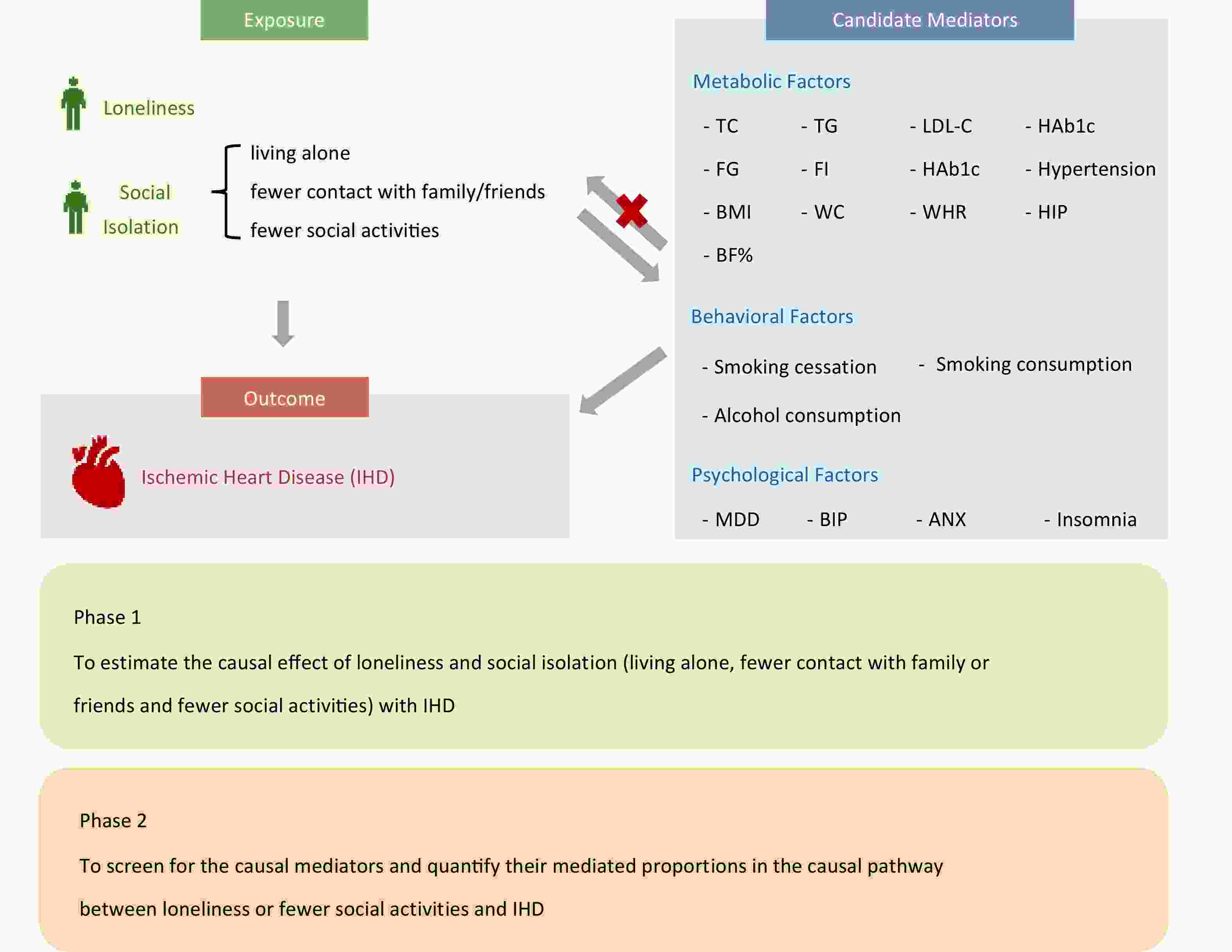
Figure 1. Overview of this study. This MR study included two phases. In phase 1, we estimated the causal association between loneliness or each of SI traits and IHD by applying bidirectional MR analyses. Loneliness and fewer social activities had a causal effect on IHD. In phase 2, we conducted network MR to screen for mediators including metabolic, behavior and psychological factors and to qualify their mediated proportions in the causal pathway from loneliness or fewer social activities to IHD. IHD, ischemic heart disease; MR, Mendelian randomization; BMI, body mass index; WHR, waist-hip ratio; WC, waist circumference; HIP, hip circumference; BF%, body fat percentage; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; FG, fasting glucose; FI, fasting insulin; HAb1c, glycated hemoglobin levels; MDD, major depressive disorder; ANX, anxiety disorder; BIP, bipolar disorder.
-
Detailed information about the data sources for exposures, candidate mediators, and outcomes in this study is summarized in Table 1.
Table 1. Detailed information of GWAS data used in the Mendelian randomization analyses
Phenotype Sample Size Ancestry Consortium/Cohort GWAS ID PMID Exposure Loneliness 487,647 European UKB NA 29970889 SI Not living alone 459,988 European UKB ukb-b-5445 NA More contact with friends or family 459,830 European UKB ukb-b-5379 NA Fewer social activities 461,369 European UKB ukb-b-5076 NA More sports club or gym 461,369 European UKB ukb-b-4000 NA More pub or social club 461,369 European UKB ukb-b-4171 NA More religious group 461,369 European UKB ukb-b-4667 NA More adult education class 461,369 European UKB ukb-b-1553 NA More other group activity 461,369 European UKB ukb-b-4077 NA Outcome IHD 184,305 Mixed CARDIoGRAMplusC4D ieu-a-7 26343387 Anthropometric factors BMI 322,154 European GIANT ieu-a-835 25673413 WHR 210,082 European GIANT ieu-a-79 25673412 WC 231,353 European GIANT ieu-a-67 25673412 HIP 211,114 European GIANT ieu-a-55 25673412 BF% 65,831 European NA ebi-a-GCST003435 26833246 Lipid factors TC 930,672 European GLGC NA 34887591 LDL-C 930,672 European GLGC NA 34887591 HDL-C 930,672 European GLGC NA 34887591 TG 930,672 European GLGC NA 34887591 Glycemic factors FG 200,622 European MAGIC ebi-a-GCST90002232 34059833 FI 151,013 European MAGIC ebi-a-GCST90002238 34059833 HAb1c 146,806 European MAGIC ebi-a-GCST90002244 34059833 Blood pressure factors Hypertension 205,694 European Finn Gen finn-b-I9_HYPTENS NA Behavioral factors* Smoking cessation 143,851 European GSCAN NA 30643251 Cigarettes per day 143,210 European GSCAN NA 30643251 Drinks per week 226,223 European GSCAN NA 30643251 Psychological factors Insomnia 217,855 European Finn Gen finn-b-F5_INSOMNIA NA MDD† 45,591 European PGC NA 29700475 ANX 10,240 European PGC NA 31712720 BIP† 353,899 European PGC NA 34002096 Note. *Summary Statistics without UKB and 23andMe were download from the GSCAN consortium (https://conservancy.umn.edu/handle/11299/201564); †Summary Statistics without UKB were download from the PFG consortium (https://pgc.unc.edu/for-researchers/download-results/). IHD, ischemic heart disease; SI, social isolation; BMI, body mass index; WHR, waist-hip ratio; WC, waist circumference; HIP, hip circumference; BF%, body fat percentage; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; FG, fasting glucose; FI, fasting insulin; HAb1c, glycated hemoglobin levels; MDD, major depressive disorder; ANX, anxiety disorder; BIP, bipolar disorder; CARDIoGRAMplusC4D, the Whole-Genome Replication and Meta-analysis of Ischemic heart disease plus Genetics of Ischemic heart disease Consortium; GIANT, the Genetic Investigation of Anthropometric Traits Consortium; EGG, the Early Growth Genetics; GLGC, the Global Lipids Genetics Consortium; UKB, UK Biobank; MAGIC, the Meta-Analyses of Glucose and Insulin-related traits Consortium; PGC, the Psychiatric Genomics Consortium; GWAS ID, id in IEU Open GWAS project; PMID, id in PubMed; MR, Mendelian randomization. -
Summary-level statistics for loneliness were obtained from a multi-trait GWAS (MTAG) in the UKB study, which included 487,647 individuals. The estimated heritability of loneliness was 4.2%[16]. Loneliness data were derived from self-reported answers via a touchscreen at the assessment center. Participants were asked, “Do you often feel lonely?” Those who answered “yes” were classified as cases, while those who responded “no” were classified as controls.
GWAS summary statistics for SI from the UKB study were extracted from the OpenGWAS platform, using the ID shown in Table 1. The evaluation of SI focused on individuals’ objective social relationships, including whether they lived alone, participated in various types of social activities, and how often they had contact with friends or family. We further analyzed different subtypes of social activities, such as participation in a sports club or gym, pub or social club, religious group, adult education classes, and other group activities. In the UKB study[17,18], each SI trait was defined by the following questionnaire items: a) “Including yourself, how many people live in your household?” Answering “one” indicated living alone. b) “How often do you visit friends or family or have them visit you?” Responses included: “no friends or family outside the household” “once a month” “once every few months” “never or almost never” “once a week” “2–4 times a week”, or “almost daily”. Answering the first four options indicated less contact with family and friends. c) “Which of the following leisure or social activities do you engage in once a week or more often?” Options were: “sports club or gym” “pub or social club” “religious group” “adult education class”, or “other group activities”. Answering “no activities mentioned above” indicated fewer social activities. SI was defined as having any of the above three traits.
-
Based on a literature review, we selected 20 candidate mediators, categorized into the following three groups, which may be implicated in the causal pathway from loneliness or SI to IHD. Metabolic factors were subdivided into anthropometric, lipid, glycemic, and blood pressure factors. Anthropometric factors analyzed in this study included body mass index (BMI)[19], waist-to-hip ratio (WHR)[20], waist circumference (WC)[20], hip circumference (HIP)[20], and body fat percentage (BF%)[21]. Lipid factors comprised total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglycerides (TG)[22]. Glycemic factors included fasting glucose (FG), fasting insulin (FI), and glycated hemoglobin levels (HbA1c) levels[23]. Blood pressure was represented by hypertension data from the Finn-Gen database.
Behavioral factors included smoking cessation, cigarettes per day, and drinks per week[24]. Psychological factors contained insomnia, major depressive disorder (MDD)[25], anxiety disorder (ANX)[26], and bipolar disorder (BIP)[27]. To avoid sample overlap between exposures and mediators, we downloaded summary-level statistics without UKB and 23andMe samples for behavioral factors from the GSCAN consortium, and data without UKB samples for MDD and BIP from the PGC consortium.
-
Nikpay M. et al. conducted a GWAS meta-analysis, which included 60,801 cases and 123,504 controls from mixed ancestry (77% European, 13% South Asian, 6% East Asian, and others from Hispanic or African American backgrounds)[28]. Case status was defined by an inclusive IHD diagnosis, encompassing MI, acute coronary syndrome, stable angina, and coronary stenosis (> 50%)[28]. Summary-level statistics for IHD can be downloaded from the CARDIoGRAMplusC4D Consortium.
-
For loneliness, we used 15 statistically independent SNPs defined by one million base-pair clumping with genome-wide significance (P < 5 × 10−8), identified by Day FR et al. as the genetic instruments[16]. For the genetic instruments of the eight SI traits and 20 candidate mediators, we implemented a series of selection and strict quality control measures.
First, to meet the assumption that instrumental variables predict the exposure, we primarily selected SNPs with genome-wide significant associations. For the eight SI traits and psychological factors, due to the limited number of SNPs reaching genome-wide significance, the P-value threshold was relaxed to P < 5 × 10−6 to ensure sufficient availability of instrument variables[29]. Clumping was performed with a cut-off of r2 < 0.01 within a window of one million base-pairs, using the 1000 Genomes European data as the reference panel to avoid linkage disequilibrium[30]. Subsequently, SNPs associated with the outcome (P < 5 × 10−8) were removed, and proxy SNPs (r2 > 0.8) were searched if SNPs could not be matched in the outcome database.
Next, we harmonized the effect of SNPs on exposure and outcome, removing palindromic SNPs with intermediate allele frequencies exceeding 0.42. To avoid potential horizontal pleiotropy, any SNP that explained more variance in the outcome than in the exposure was excluded using the Steiger filtering method. Outliers were then removed using the RadialMR method. F-statistics were used to estimate the strength of the genetic instruments, and only instruments with an F-statistic greater than ten were retained for subsequent statistical analysis to avoid the inclusion of weak instruments.
-
In Phase 1, we applied two-sample MR to assess the bidirectional causal effect of loneliness and each SI trait on IHD. All MR analyses fulfilled three core assumptions: (1) the genetic variants must be strongly associated with the exposure; (2) the genetic variants must not be associated with confounders of the associations between each exposure and the outcome; and (3) the genetic variants must not affect the outcome independently of the exposure[13,31]. For each pair of relationships between exposure and outcome, the causal effects were estimated using the inverse variance weighted (IVW) method, which combined the Wald ratio estimates of each SNP[32]. This method provides the highest precision and maintains maximum power, assuming the SNPs satisfy the MR assumptions[33].
-
In Phase 2, for significant associations identified in Phase 1, we performed network MR analyses to assess mediation[14]. In the first step, we explored the causality between the exposure and candidate mediators using a bidirectional MR approach. Specifically, if a causal relationship was found between the exposure and candidate mediators, with no reverse relationship, the candidate mediator was included in the next step; otherwise, the candidate mediator was removed. In the second step, genetic instruments for the candidate mediators were used to estimate their causal effect on IHD using the IVW method.
Where there was evidence that poor social health influenced the candidate mediator, which in turn affected IHD, we considered the candidate mediator to be part of the causal pathway. The “product of coefficients” method was applied to estimate the indirect effect of the exposure on the outcome via each mediator, specifically by multiplying the β coefficients from the two steps[34]. The mediated proportion of each mediator was calculated by dividing the indirect effect by the total effect obtained from the two-sample MR in Phase 1. Standard errors were derived using the delta method[35].
-
To validate the robustness of the IVW results, we conducted a series of sensitivity analyses. First, we applied the Weighted Median (WM) method, which requires that at least 50% of the weight comes from valid instrumental variables to provide a consistent estimate[36]. If no heterogeneity and pleiotropy were detected, the IVW results were preferred. Second, the MR Egger method was used to assess bias due to horizontal pleiotropy based on its intercept term. An intercept not equal to zero (P < 0.05) indicated the presence of horizontal pleiotropy bias[37]. Third, the presence of pleiotropy was further evaluated using the MR Pleiotropy Residual Sum and Outlier method (MR-PRESSO), which detects potentially pleiotropic outliers and corrects horizontal pleiotropy by removing them[38]. Fourth, a leave-one-out analysis was performed to assess the influence of individual variants on the observed associations by removing each SNP in turn[39]. Finally, Cochran’s Q statistic was used to quantify heterogeneity, with a P-value < 0.05 considered statistically significant.
We used the Benjamini–Hochberg procedure to correct for multiple testing, with a false discovery rate (FDR)-adjusted P-value of less than 0.05 indicating statistical significance. In bidirectional two-sample MR, 18 corrections were applied when analyzing the relationships between loneliness or SI and IHD. In network MR analyses, we reported adjusted P-values corrected for 20 tests (20 candidate mediators) in the first step, while unadjusted P-values were reported for the second step to avoid overcorrection.
In this study, results were presented as odds ratios (OR), β coefficients, or proportions, with corresponding 95% CIs. All analyses were performed using the R packages “RadialMR”, “TwoSampleMR”, and “MR-PRESSO” in R software (version 4.1.2).
-
Two-sample MR results using the IVW method showed a causal relationship between loneliness and IHD (OR = 2.129; 95% CI: 1.380 to 3.285). For SI traits, fewer social activities led to an increased risk of IHD (OR = 1.815; 95% CI: 1.189 to 2.772), while living alone and contact with friends or family were not associated with IHD (Table 2). Among the five subtypes of social activities, only increased participation in sports club or gym activities had a protective effect on IHD (OR = 0.333; 95% CI: 0.204 to 0.542). The F-statistics of SNPs selected for MR analyses were all above 10, and more detailed information on SNPs is shown in Supplementary Table S1.
Table 2. Two-sample Mendelian randomization estimates for the causal associations of loneliness or social isolation with IHD
Exposure Method N_SNP OR (95% CI) q-value Loneliness IVW 12 2.129 (1.380, 3.285) 0.003 WM 2.515 (1.452, 4.355) 0.017 Living alone IVW 19 0.728 (0.396, 1.339) 0.346 WM 0.587 (0.251, 1.371) 0.307 Contact with friends or family IVW 105 0.876 (0.751, 1.023) 0.154 WM 0.935 (0.750, 1.165) 0.618 Fewer social activities IVW 89 1.815 (1.189, 2.772) 0.017 WM 1.646 (0.913, 2.968) 0.205 - More sports club or gym IVW 67 0.333 (0.204, 0.542) < 0.001 WM 0.428 (0.216, 0.850) 0.085 - More pub or social club IVW 90 0.321 (0.188, 0.546) 0.073 WM 0.399 (0.185, 0.859) 0.130 - More religious group IVW 151 0.663 (0.437, 1.005) 0.119 WM 0.641 (0.353, 1.165) 0.261 - More adult education class IVW 30 0.625 (0.154, 2.545) 0.542 WM 2.702 (0.366, 19.925) 0.424 - More other group activities IVW 51 0.540 (0.282, 1.032) 0.124 WM 1.285 (0.495, 3.336) 0.641 Note. All statistical tests were two-sided. q-value < 0.05 was considered significant. IHD, ischemic heart disease; IVW, inverse variance weighted method; WM, weighted median method; N_SNP, number of SNPS; q-value, P value corrected by False Discovery Rate method. The effect estimates were similar when using the WM method, although they were not statistically significant for fewer social activities and sports. Due to the absence of heterogeneity in all analyses (Supplementary Table S2), we prioritized the IVW results. Pleiotropy was only observed for sports in the intercept of the MR Egger test, but in the MR-PRESSO analysis, no outliers contributing to horizontal pleiotropy were observed (Supplementary Table S2). Furthermore, leave-one-out analyses revealed that no single SNP influenced the results (Supplementary Table S2).
In the reverse direction, no evidence indicated causal associations of genetically predicted IHD with each exposure using the IVW method, and sensitivity analyses confirmed that the results were robust (Supplementary Tables S3–S4).
-
Based on the two-sample MR results, we conducted network MR analyses to investigate the mediating pathway from loneliness or fewer social activities to IHD via 20 modifiable risk factors.
In the first step of the network MR analysis, the effects of genetically predicted loneliness on each candidate mediator using the IVW method are shown in Table 3. Among the 20 candidate mediators, increased loneliness was associated with higher WHR (β = 0.301; 95% CI: 0.128 to 0.475), WC (β = 0.262; 95% CI: 0.065 to 0.460), BF% (β = 0.339; 95% CI: 0.082 to 0.597), TC (β, 0.113; 95% CI: 0.036 to 0.190), TG (β = 0.170; 95% CI: 0.086 to 0.255), LDL-C (β = 0.147; 95% CI: 0.069 to 0.224), and MDD (OR = 2.439; 95% CI: 1.550 to 3.838) (Figure 2A). Reverse MR analyses showed a causal effect of TG with loneliness, leading to the exclusion of TG (Supplementary Table S5). Although reverse MR analyses also showed an association between LDL-C and loneliness, the result was largely driven by horizontal pleiotropy (P for Egger intercept = 0.001; Supplementary Table S5). In the second step, we assessed the causal effect of six candidate mediators on IHD using genetic instruments without weak bias (Supplementary Table S6). Figure 2B indicated that WHR, BF%, TC, and LDL-C were positively associated with IHD.
Table 3. Two-sample Mendelian randomization estimates for the causal associations of loneliness or social isolation with 20 candidate mediators
Candidate mediators Exposure N_SNP β (95% CI) OR (95% CI) q-value Anthropometric factors BMI Loneliness 10 0.086 (−0.113, 0.285) − 0.496 Fewer social activities 53 0.145 (−0.071, 0.362) − 0.297 WHR Loneliness 14 0.301 (0.128, 0.475) − 0.003 Fewer social activities 64 0.199 (−0.033, 0.432) − 0.233 WC Loneliness 12 0.262 (0.065, 0.460) − 0.028 Fewer social activities 62 0.039 (−0.182, 0.260) − 0.766 HIP Loneliness 11 −0.110 (−0.316, 0.097) − 0.397 Fewer social activities 58 −0.160 (−0.402, 0.081) − 0.297 BF% Loneliness 12 0.339 (0.082, 0.597) − 0.028 Fewer social activities 59 0.163 (−0.139, 0.466) − 0.392 Lipid Factors TC Loneliness 10 0.113 (0.036, 0.190) − 0.016 Fewer social activities 69 0.042 (−0.037, 0.122) − 0.392 LDL-C Loneliness 11 0.147 (0.069, 0.224) − 0.001 Fewer social activities 70 0.099 (0.017, 0.181) − 0.850 HDL-C Loneliness 6 −0.065 (−0.178, 0.049) − 0.377 Fewer social activities 57 −0.292 (−0.382, -0.202) − < 0.001 TG Loneliness 9 0.170 (0.086, 0.255) − 0.001 Fewer social activities 57 0.279 (0.187, 0.371) − < 0.001 Glycemic factors FG Loneliness 14 0.030 (−0.049, 0.110) − 0.535 Fewer social activities 84 −0.061 (−0.146, 0.024) − 0.293 FI Loneliness 13 0.069 (−0.023, 0.161) − 0.219 Fewer social activities 85 0.126 (0.029, 0.222) − 0.037 HbA1c Loneliness 14 0.048 (−0.010, 0.106) − 0.172 Fewer social activities 85 0.019 (−0.045, 0.082) − 0.659 Lipid factors Hypertension Loneliness 14 − 1.059 (0.720, 1.556) 0.774 Fewer social activities 80 − 1.782 (1.151, 2.757) 0.037 Behavioral factors Smoking cessation Loneliness 14 − 0.719 (0.525, 0.985) 0.089 Fewer social activities 83 − 0.566 (0.401, 0.799) 0.008 Cigarettes per day Loneliness 13 −0.197 (−0.375, -0.020) − 0.074 Fewer social activities 91 −0.132 (−0.294, 0.030) − 0.245 Drinks per week Loneliness 13 0.126 (−0.001, 0.252) − 0.102 Fewer social activities 74 0.208 (0.065, 0.350) − 0.021 Psychological factors Insomnia Loneliness 15 − 1.446 (0.359, 5.818) 0.571 Fewer social activities 92 − 0.556 (0.118, 2.612) 0.600 MDD Loneliness 12 − 2.440 (1.550, 3.838) 0.001 Fewer social activities 67 − 1.408 (0.882, 2.248) 0.290 ANX Loneliness 11 − 1.730 (0.306, 9.786) 0.595 Fewer social activities 45 − 1.706 (0.172, 16.878) 0.720 BIP Loneliness 13 − 1.662 (0.919, 3.004) 0.169 Fewer social activities 60 − 0.573 (0.343, 0.958) 0.096 Note. All statistical tests were two-sided. q-value < 0.05 was considered significant. BMI, body mass index; WHR, waist-hip ratio; WC, waist circumference; HIP, hip circumference; BF%, body fat percentage; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; FG, fasting glucose; FI, fasting insulin; HAb1c, glycated hemoglobin levels; MDD, major depressive disorder; ANX, anxiety disorder; BIP, bipolar disorder; N_SNP, number of SNPS; q-value, P value corrected by False Discovery Rate method. 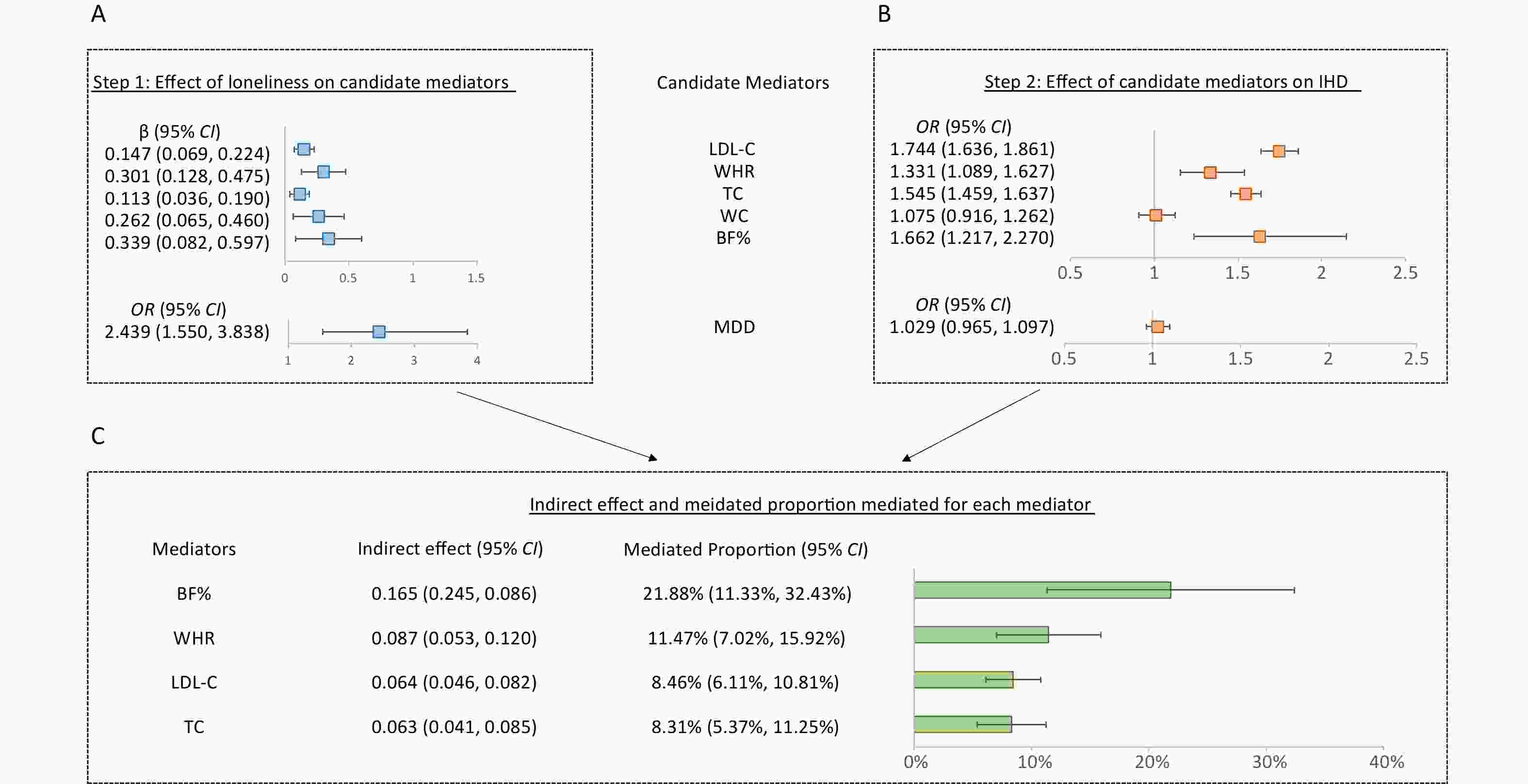
Figure 2. Network Mendelian randomization analyses of the effect of loneliness on IHD via candidate mediators. A, the first step in network MR analyses estimated the causal effect of loneliness on candidate mediators. B, the second step in network MR estimated the causal effect of candidate mediators on IHD. C, Indirect effects of exposure on outcome via each mediator was computed by “product of coefficients” method, and 95% CI was calculated by delta method. MR estimates were derived from the IVW method. The results were presented as ORs, β coefficients or proportions, with corresponding 95% CIs. The squares represented ORs or β coefficients, and the bars represented proportions, with the error bars indicating 95% CIs. All statistical tests were two-sided. IHD, ischemic heart disease; LDL-C, low-density lipoprotein cholesterol; WHR, waist-hip ratio; TC, total cholesterol; WC, waist circumference; BF%, body fat percentage; MDD, major depressive disorder.
According to the results of all sensitivity analyses, the IVW results of the network analyses were robust (Supplementary Tables S5, S7–S8). The P-values from Cochran’s Q test were all greater than 0.05, indicating no heterogeneity. MR-Egger intercept analyses showed no pleiotropy (P > 0.05). Additionally, the MR-PRESSO method did not detect any potentially pleiotropic outliers, except for BIP; however, the distortion test showed no influence of outliers on the association between loneliness and BIP (P > 0.05). The leave-one-out method revealed that no single SNP had a significant influence on the results.
Therefore, we identified BF%, WHR, TC, and LDL-C as mediators in the causal pathway from loneliness to IHD (Figure 2C). The largest causal mediator was BF% (proportion, 21.88%; 95% CI: 11.33% to 32.43%), followed by WHR (proportion, 11.47%; 95% CI: 6.87% to 16.07%), TC (proportion, 8.31%; 95% CI: 5.37% to 11.25%), and LDL-C (proportion, 8.46%; 95% CI: 6.11% to 10.81%).
-
First, the causal estimates between genetically predicted fewer social activities and 20 candidate mediators using the IVW method are shown in Table 3. Figure 3A indicates that genetically predicted fewer social activities were significantly positively associated with four candidate mediators: drinks per week (β = 0.208; 95% CI: 0.065 to 0.35), TG (β = 0.279; 95% CI: 0.187 to 0.371), hypertension (OR = 1.782; 95% CI: 1.151 to 2.757), and FI (β = 0.126; 95% CI: 0.029 to 0.222). Additionally, it was significantly negatively associated with smoking cessation (OR = 0.566; 95% CI: 0.401 to 0.799) and HDL-C (β = −0.292; 95% CI: −0.382 to −0.202). A bidirectional causality was observed between drinks per week and fewer social activities (Supplementary Table S9).
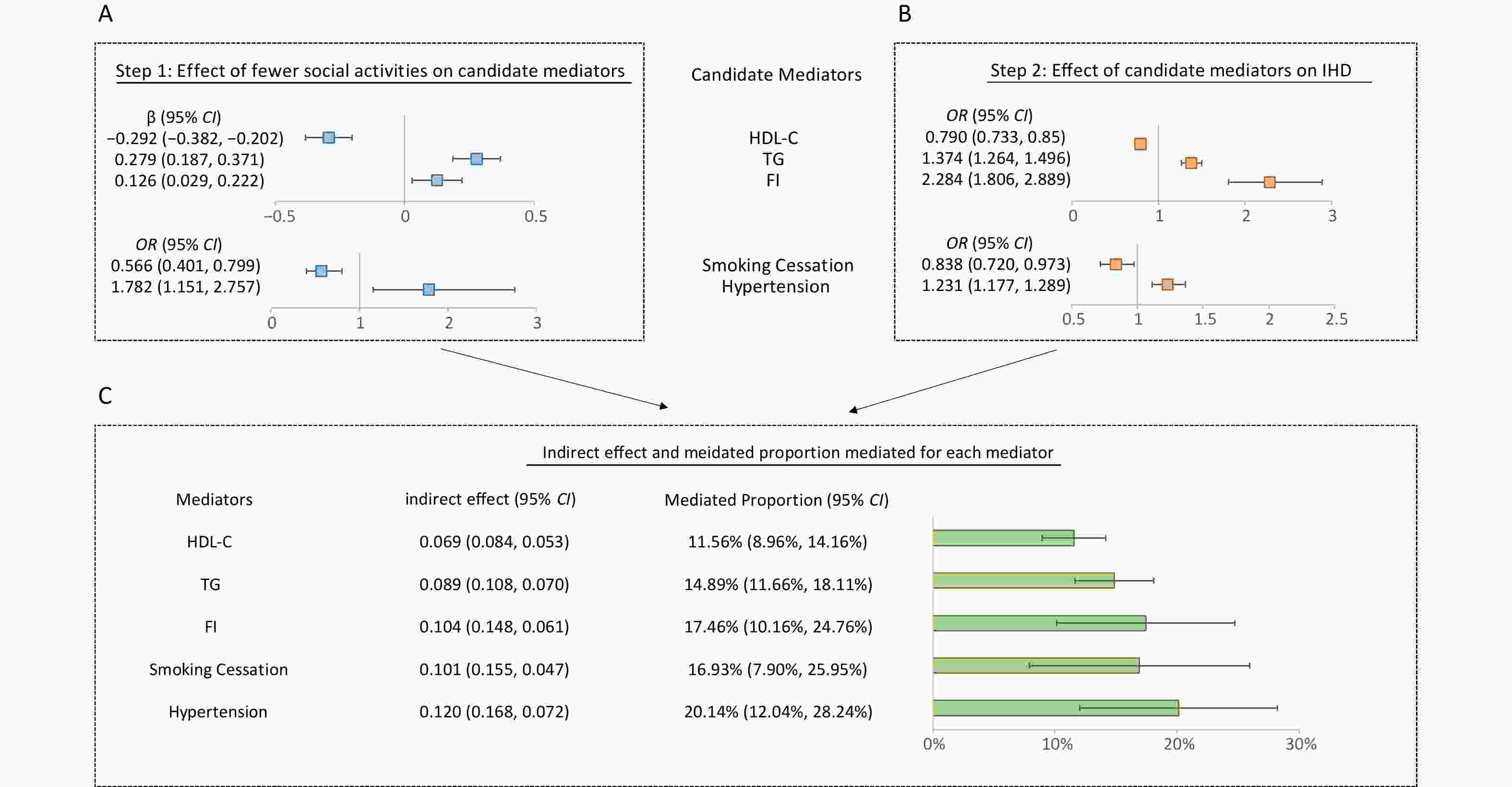
Figure 3. Network Mendelian randomization analyses of the effect of fewer social activities on IHD via candidate mediators. A, the first step in network MR estimated the causal effect of fewer social activities on candidate mediators. B, the second step in network MR estimated the causal effect of candidate mediators on IHD. C, indirect effects of exposure on outcome via each mediator was computed by “product of coefficients” method, and 95% CI was calculated by delta method. MR estimates were derived from the IVW method. The results were presented as ORs, β coefficients or proportions, with corresponding 95% CIs. The squares represented ORs or β coefficients, and the bars represented proportions, with the error bars indicating 95% CIs. All statistical tests were two-sided. IHD, ischemic heart disease; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; FI, fasting insulin.
Therefore, the second step included five candidate mediators, with summary information on genome-wide significant SNPs listed in Supplementary Table S10. IVW results of the second step in network analyses were displayed in Figure 3B. Compared to current smoking, smoking cessation had a protective effect on the risk of IHD. Notably, higher HDL-C was associated with a decreased risk of IHD, while hypertension and 1 SD higher FI were associated with an increased risk of IHD.
The sensitivity analysis results were shown in Supplementary Tables S9, S11–S12. Heterogeneity, evaluated by Cochran’s Q test, was not observed. Although pleiotropy was observed in the causal relationship between hypertension and IHD, the P-value of the MR-PRESSO distortion tests was greater than 0.05, indicating that outliers did not have a statistically significant impact on the results. Leave-one-out analyses confirmed that no single SNP had a strong influence on the estimated effects.
Finally, HDL-C, TG, FI, smoking cessation, and hypertension were identified as mediators in the causal pathway from fewer social activities to IHD. Figure 3C displayed the indirect effect and mediated proportion explained by each mediator. For fewer social activities leading to IHD, the mediated proportions ranged from 11.56% (95% CI: 8.96% to 14.16%) for HDL-C to 20.14% (95% CI: 12.04% to 28.23%) for hypertension.
-
According to available literature, this is the first study focusing on the causal association between poor social health and IHD using MR analyses, examining subjective emotional loneliness and objective SI separately. Our evidence indicates that loneliness or reduced social activities are causally associated with an increased risk of IHD, deepening our understanding of IHD etiology. Furthermore, we identified key mediators in the causal pathway, which are critical for guiding prevention and intervention strategies to mitigate IHD risk attributed to poor social health. Among 20 modifiable candidate mediators, four factors mediated the association between loneliness and IHD, ranked by mediated proportion as BF%, WHR, LDL-C, and TC. However, in the causal pathway from fewer social activities to IHD, hypertension, FI, smoking cessation, TG, and HDL-C were identified as mediators.
Although epidemiological studies have reported an association between loneliness or SI and IHD, the results have been inconsistent, potentially due to confounding factors[40,41]. Our findings are the first to establish a causal relationship between loneliness and IHD. Previous studies have shown that loneliness may activate the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system, which can lead to atherosclerosis and subsequently increase the risk of IHD[42]. Prior studies have also demonstrated that increased feelings of loneliness are linked to elevated levels of various inflammatory markers, including interleukin-6, tumor necrosis factor-alpha, interleukin-1 beta, and monocyte chemoattractant protein[43,44]. Increased levels of these inflammation markers, released during aversive stimulation such as stress and loneliness, are associated with CVD[45,46].
Diverging from previous holistic studies on SI[41], and facilitated by the UKB database, we conducted further assessment to explore the association between each trait of SI and IHD separately. This provides evidence for determining the priority intervention order for different traits in socially isolated populations, particularly those with multiple manifestations. Our findings suggest a positive causal relationship between fewer social activities and IHD, whereas living alone and contact with friends or family did not show such an association. Compared to living with others and engaging in communication with friends or family, participating in more social activities reflects a broader social network and greater social interactions. Therefore, fewer social activities are strongly linked to adverse health outcomes. A national prospective study in Finland provided similar evidence that living alone did not display any statistically significant effect on MI incidence risk and suggested that the association between living alone and MI observed in previous studies may be explained by socioeconomic factors, such as education, occupation, income, and employment status[47].
Additionally, we explored the differential association of various social activities with IHD risk. Our findings of no relationship between participation in religious groups, adult education classes, or pub or social clubs and IHD align with previous studies[48,49]. Only participation in sports clubs or gyms was correlated with significant risk reductions in IHD. This distinction may be attributed to the multifaceted nature of sports clubs or gyms. Exercise in such settings not only increases interaction with other members of society but also improves cardiopulmonary function, which is known to be effective in preventing IHD[50].
Bidirectional MR results revealed that genetically predicted IHD does not directly lead to poor social health. However, due to factors such as long-term treatment and reduced income, feelings of loneliness and SI are common among IHD patients, contributing to poorer prognosis and higher mortality rates[51]. Therefore, addressing mental health remains essential in the treatment and management of IHD patients.
Notably, this study identified and quantified the mediating roles of modifiable factors in the causal pathway. Utilizing the available database, we selected 20 candidate mediators, comprehensively covering metabolic, behavioral, and psychological factors. In the causal pathway from loneliness to IHD, BF% and WHR played important mediating roles. Previous epidemiological studies have demonstrated that loneliness impacts dietary behaviors, which play a key role in triggering and maintaining obesity, a well-established traditional risk factor for IHD[52]. Inferior to adiposity traits, LDL-C and TC mediated 8.46% and 8.31% of the causal pathway, respectively. Our findings support the neuroendocrine hypothesis proposed by Cacioppo et al., which suggests that loneliness is typically associated with increased stress and higher levels of HPA axis activation, resulting in excessive cortisol that affects lipid metabolism, thereby increasing LDL-C and TC levels[53,54].
For behavioral factors, we found no clear evidence establishing a causal relationship between loneliness and smoking or drinks per week, which is generally consistent with the results of a previous MR study[55]. Additionally, our results revealed no causality between genetically predicted MDD and IHD, suggesting that the significant associations observed in observational studies may be partly influenced by residual confounding or reverse causal bias[56]. Therefore, interventions and control measures targeting obesity and lipid disorders may be effective in reducing IHD risk among individuals experiencing loneliness.
In the causal pathway from fewer social activities to IHD, the mediating factors were different, including hypertension, FI, TG, HDL-C, and smoking cessation. The most significant mediator was hypertension, whose mediating effect may be explained by oxidative stress, a key molecular mechanism linking SI to CVD[57]. In socially isolated animals, oxidative stress in the brain increases sympathetic outflow and raises blood pressure, while oxidative stress in peripheral vascular tissue increases vascular tone, promotes atherogenesis, and leads to elevated blood pressure[58]. Insulin resistance or hyperinsulinism causes peripheral vasoconstriction or lipid imbalance, and low HDL-C and high TG lead to endothelial dysfunction and promote the formation of atherosclerotic plaques, which may partly explain the mediating effects of high insulin, low HDL-C, and high TG[59,60]. However, it should be noted that an MR study found a reciprocal causal effect among TG, HDL-C and FI, so the proportion mediated by these mediators may overlap in our analysis[61]. Our results also supported the notion that SI increases the difficulty of smoking cessation and thus elevates the risk of IHD, consistent with current observational evidence[62]. Meanwhile, drinks per week were excluded from our mediation analysis due to their bidirectional causal associations with fewer social activities. For socially isolated individuals, it is important to focus on metabolic indicators and smoking cessation to reduce the risk of IHD.
This MR study provides novel evidence for the causal impact of poor social health on IHD and identifies causal mediators in the pathway. This work has several strengths. First, to avoid pleiotropy and heterogeneity, we set rigorous screening criteria for genetic instruments, and the results of multiple sensitivity analyses supported the robustness of the IVW results. Second, we applied strict criteria for selecting mediators to avoid reverse causality and ensure the credibility of the mediation analyses.
However, there are some limitations in this study. First, the mediators of loneliness or fewer social activities on IHD cannot be fully explored. On one hand, to avoid bias due to sample overlap in two-sample MR analyses, several potential mediators were not included in our mediation analysis, such as physical activity, coffee consumption, and dietary habits. On the other hand, the MR method is only appropriate for risk factors with suitable genetic instrumental variables. Several potential mediators, such as health awareness and poverty, are not heritable and, therefore, unsuitable for MR analysis. Furthermore, recent research has identified emerging factors, such as gut microbiota and circadian rhythm disturbances, which may also play significant roles in cardiovascular health[63,64]. In the future, incorporating these emerging risk factors may contribute to a more comprehensive understanding of the pathway linking poor social health to cardiovascular outcomes. Second, the proportion mediated by each mediator may overlap due to possible interrelations between mediators. Third, a key limitation of the MR method is the potential for pleiotropy, where the genetic variants used may affect the outcome through pathways unrelated to the exposure of interest. This can introduce bias and compromise the accuracy of causal estimates. Since several MR assumptions are untestable, the results should be interpreted with caution. However, in this study, we implemented strict criteria for selecting instrumental variables and conducted quality control to ensure that the selected SNPs aligned with the core assumptions. Additionally, a series of sensitivity analyses indicated that horizontal pleiotropy and outliers did not affect our results. Fourth, ethnic differences can influence the performance of cardiovascular risk prediction models, highlighting the importance of ethnic diversity in cardiovascular research[65]. For example, the Pooled Cohort Equations reported in the American College of Cardiology/American Heart Association guidelines did not perform well when applied to East Asian populations[66]. The heterogeneity in the association between genetic variants and phenotypic traits across different ethnic groups may lead to biased effect estimates, as these genetic variants may not effectively randomize confounding factors when used as instrumental variables in diverse populations[67]. Due to the lack of large-scale GWAS data on loneliness and SI in other ethnic groups, this study focused on European populations in high-income countries. Therefore, we encourage future studies to assess whether our findings can be replicated in other ethnic groups or in low- and middle-income countries.
-
Our MR analyses elucidated the detrimental causal effect of loneliness and SI, particularly due to fewer social activities, on the risk of IHD and identified key mediators in the causal pathway. These findings suggest that loneliness and fewer social engagement should be considered when developing strategies for IHD prevention and reducing the overall disease burden. Furthermore, for individuals experiencing loneliness or limited social activities, comprehensive interventions targeting metabolic factors and promoting healthier lifestyles may be effective in reducing IHD risk.
doi: 10.3967/bes2024.170
Association of Loneliness and Social Isolation with Ischemic Heart Disease: A Bidirectional and Network Mendelian Randomization Study
-
Abstract:
Objective Observational studies have shown inconsistent associations of loneliness or social isolation (SI) with ischemic heart disease (IHD), with unknown mediators. Methods Using data from genome-wide association studies of predominantly European ancestry, we performed a bidirectional two-sample Mendelian Randomization (MR) study to estimate causal effects of loneliness (N = 487,647) and SI traits on IHD (N = 184,305). SI traits included whether individuals lived alone, participated in various types of social activities, and how often they had contact with friends or family (N = 459,830 to 461,369). A network MR study was conducted to evaluate the mediating roles of 20 candidate mediators, including metabolic, behavioral and psychological factors. Results Loneliness increased IHD risk (OR = 2.129; 95% confidence interval [CI]: 1.380 to 3.285), mediated by body fat percentage, waist-hip ratio, total cholesterol, and low-density lipoprotein cholesterol. For SI traits, only fewer social activities increased IHD risk (OR = 1.815; 95% CI: 1.189 to 2.772), mediated by hypertension, high-density lipoprotein cholesterol, triglycerides, fasting insulin, and smoking cessation. No reverse causality of IHD with loneliness and SI was found. Conclusion These findings suggested more attention should be paid to individuals who feel lonely and have fewer social activities to prevent IHD, with several mediators as prioritized targets for intervention. -
Key words:
- Mendelian randomization /
- Loneliness /
- Social isolation /
- Ischemic heart disease /
- Mediation analyses
The authors declare that they have no competing interests.
Ethical informed consent and approval were completed in the original study, so no additional ethical approval or informed consent was required.
注释:1) Authors’ Contributions: 2) Competing Interests: 3) Ethics: -
Figure 1. Overview of this study. This MR study included two phases. In phase 1, we estimated the causal association between loneliness or each of SI traits and IHD by applying bidirectional MR analyses. Loneliness and fewer social activities had a causal effect on IHD. In phase 2, we conducted network MR to screen for mediators including metabolic, behavior and psychological factors and to qualify their mediated proportions in the causal pathway from loneliness or fewer social activities to IHD. IHD, ischemic heart disease; MR, Mendelian randomization; BMI, body mass index; WHR, waist-hip ratio; WC, waist circumference; HIP, hip circumference; BF%, body fat percentage; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; FG, fasting glucose; FI, fasting insulin; HAb1c, glycated hemoglobin levels; MDD, major depressive disorder; ANX, anxiety disorder; BIP, bipolar disorder.
Figure 2. Network Mendelian randomization analyses of the effect of loneliness on IHD via candidate mediators. A, the first step in network MR analyses estimated the causal effect of loneliness on candidate mediators. B, the second step in network MR estimated the causal effect of candidate mediators on IHD. C, Indirect effects of exposure on outcome via each mediator was computed by “product of coefficients” method, and 95% CI was calculated by delta method. MR estimates were derived from the IVW method. The results were presented as ORs, β coefficients or proportions, with corresponding 95% CIs. The squares represented ORs or β coefficients, and the bars represented proportions, with the error bars indicating 95% CIs. All statistical tests were two-sided. IHD, ischemic heart disease; LDL-C, low-density lipoprotein cholesterol; WHR, waist-hip ratio; TC, total cholesterol; WC, waist circumference; BF%, body fat percentage; MDD, major depressive disorder.
Figure 3. Network Mendelian randomization analyses of the effect of fewer social activities on IHD via candidate mediators. A, the first step in network MR estimated the causal effect of fewer social activities on candidate mediators. B, the second step in network MR estimated the causal effect of candidate mediators on IHD. C, indirect effects of exposure on outcome via each mediator was computed by “product of coefficients” method, and 95% CI was calculated by delta method. MR estimates were derived from the IVW method. The results were presented as ORs, β coefficients or proportions, with corresponding 95% CIs. The squares represented ORs or β coefficients, and the bars represented proportions, with the error bars indicating 95% CIs. All statistical tests were two-sided. IHD, ischemic heart disease; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; FI, fasting insulin.
Table 1. Detailed information of GWAS data used in the Mendelian randomization analyses
Phenotype Sample Size Ancestry Consortium/Cohort GWAS ID PMID Exposure Loneliness 487,647 European UKB NA 29970889 SI Not living alone 459,988 European UKB ukb-b-5445 NA More contact with friends or family 459,830 European UKB ukb-b-5379 NA Fewer social activities 461,369 European UKB ukb-b-5076 NA More sports club or gym 461,369 European UKB ukb-b-4000 NA More pub or social club 461,369 European UKB ukb-b-4171 NA More religious group 461,369 European UKB ukb-b-4667 NA More adult education class 461,369 European UKB ukb-b-1553 NA More other group activity 461,369 European UKB ukb-b-4077 NA Outcome IHD 184,305 Mixed CARDIoGRAMplusC4D ieu-a-7 26343387 Anthropometric factors BMI 322,154 European GIANT ieu-a-835 25673413 WHR 210,082 European GIANT ieu-a-79 25673412 WC 231,353 European GIANT ieu-a-67 25673412 HIP 211,114 European GIANT ieu-a-55 25673412 BF% 65,831 European NA ebi-a-GCST003435 26833246 Lipid factors TC 930,672 European GLGC NA 34887591 LDL-C 930,672 European GLGC NA 34887591 HDL-C 930,672 European GLGC NA 34887591 TG 930,672 European GLGC NA 34887591 Glycemic factors FG 200,622 European MAGIC ebi-a-GCST90002232 34059833 FI 151,013 European MAGIC ebi-a-GCST90002238 34059833 HAb1c 146,806 European MAGIC ebi-a-GCST90002244 34059833 Blood pressure factors Hypertension 205,694 European Finn Gen finn-b-I9_HYPTENS NA Behavioral factors* Smoking cessation 143,851 European GSCAN NA 30643251 Cigarettes per day 143,210 European GSCAN NA 30643251 Drinks per week 226,223 European GSCAN NA 30643251 Psychological factors Insomnia 217,855 European Finn Gen finn-b-F5_INSOMNIA NA MDD† 45,591 European PGC NA 29700475 ANX 10,240 European PGC NA 31712720 BIP† 353,899 European PGC NA 34002096 Note. *Summary Statistics without UKB and 23andMe were download from the GSCAN consortium (https://conservancy.umn.edu/handle/11299/201564); †Summary Statistics without UKB were download from the PFG consortium (https://pgc.unc.edu/for-researchers/download-results/). IHD, ischemic heart disease; SI, social isolation; BMI, body mass index; WHR, waist-hip ratio; WC, waist circumference; HIP, hip circumference; BF%, body fat percentage; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; FG, fasting glucose; FI, fasting insulin; HAb1c, glycated hemoglobin levels; MDD, major depressive disorder; ANX, anxiety disorder; BIP, bipolar disorder; CARDIoGRAMplusC4D, the Whole-Genome Replication and Meta-analysis of Ischemic heart disease plus Genetics of Ischemic heart disease Consortium; GIANT, the Genetic Investigation of Anthropometric Traits Consortium; EGG, the Early Growth Genetics; GLGC, the Global Lipids Genetics Consortium; UKB, UK Biobank; MAGIC, the Meta-Analyses of Glucose and Insulin-related traits Consortium; PGC, the Psychiatric Genomics Consortium; GWAS ID, id in IEU Open GWAS project; PMID, id in PubMed; MR, Mendelian randomization. Table 2. Two-sample Mendelian randomization estimates for the causal associations of loneliness or social isolation with IHD
Exposure Method N_SNP OR (95% CI) q-value Loneliness IVW 12 2.129 (1.380, 3.285) 0.003 WM 2.515 (1.452, 4.355) 0.017 Living alone IVW 19 0.728 (0.396, 1.339) 0.346 WM 0.587 (0.251, 1.371) 0.307 Contact with friends or family IVW 105 0.876 (0.751, 1.023) 0.154 WM 0.935 (0.750, 1.165) 0.618 Fewer social activities IVW 89 1.815 (1.189, 2.772) 0.017 WM 1.646 (0.913, 2.968) 0.205 - More sports club or gym IVW 67 0.333 (0.204, 0.542) < 0.001 WM 0.428 (0.216, 0.850) 0.085 - More pub or social club IVW 90 0.321 (0.188, 0.546) 0.073 WM 0.399 (0.185, 0.859) 0.130 - More religious group IVW 151 0.663 (0.437, 1.005) 0.119 WM 0.641 (0.353, 1.165) 0.261 - More adult education class IVW 30 0.625 (0.154, 2.545) 0.542 WM 2.702 (0.366, 19.925) 0.424 - More other group activities IVW 51 0.540 (0.282, 1.032) 0.124 WM 1.285 (0.495, 3.336) 0.641 Note. All statistical tests were two-sided. q-value < 0.05 was considered significant. IHD, ischemic heart disease; IVW, inverse variance weighted method; WM, weighted median method; N_SNP, number of SNPS; q-value, P value corrected by False Discovery Rate method. Table 3. Two-sample Mendelian randomization estimates for the causal associations of loneliness or social isolation with 20 candidate mediators
Candidate mediators Exposure N_SNP β (95% CI) OR (95% CI) q-value Anthropometric factors BMI Loneliness 10 0.086 (−0.113, 0.285) − 0.496 Fewer social activities 53 0.145 (−0.071, 0.362) − 0.297 WHR Loneliness 14 0.301 (0.128, 0.475) − 0.003 Fewer social activities 64 0.199 (−0.033, 0.432) − 0.233 WC Loneliness 12 0.262 (0.065, 0.460) − 0.028 Fewer social activities 62 0.039 (−0.182, 0.260) − 0.766 HIP Loneliness 11 −0.110 (−0.316, 0.097) − 0.397 Fewer social activities 58 −0.160 (−0.402, 0.081) − 0.297 BF% Loneliness 12 0.339 (0.082, 0.597) − 0.028 Fewer social activities 59 0.163 (−0.139, 0.466) − 0.392 Lipid Factors TC Loneliness 10 0.113 (0.036, 0.190) − 0.016 Fewer social activities 69 0.042 (−0.037, 0.122) − 0.392 LDL-C Loneliness 11 0.147 (0.069, 0.224) − 0.001 Fewer social activities 70 0.099 (0.017, 0.181) − 0.850 HDL-C Loneliness 6 −0.065 (−0.178, 0.049) − 0.377 Fewer social activities 57 −0.292 (−0.382, -0.202) − < 0.001 TG Loneliness 9 0.170 (0.086, 0.255) − 0.001 Fewer social activities 57 0.279 (0.187, 0.371) − < 0.001 Glycemic factors FG Loneliness 14 0.030 (−0.049, 0.110) − 0.535 Fewer social activities 84 −0.061 (−0.146, 0.024) − 0.293 FI Loneliness 13 0.069 (−0.023, 0.161) − 0.219 Fewer social activities 85 0.126 (0.029, 0.222) − 0.037 HbA1c Loneliness 14 0.048 (−0.010, 0.106) − 0.172 Fewer social activities 85 0.019 (−0.045, 0.082) − 0.659 Lipid factors Hypertension Loneliness 14 − 1.059 (0.720, 1.556) 0.774 Fewer social activities 80 − 1.782 (1.151, 2.757) 0.037 Behavioral factors Smoking cessation Loneliness 14 − 0.719 (0.525, 0.985) 0.089 Fewer social activities 83 − 0.566 (0.401, 0.799) 0.008 Cigarettes per day Loneliness 13 −0.197 (−0.375, -0.020) − 0.074 Fewer social activities 91 −0.132 (−0.294, 0.030) − 0.245 Drinks per week Loneliness 13 0.126 (−0.001, 0.252) − 0.102 Fewer social activities 74 0.208 (0.065, 0.350) − 0.021 Psychological factors Insomnia Loneliness 15 − 1.446 (0.359, 5.818) 0.571 Fewer social activities 92 − 0.556 (0.118, 2.612) 0.600 MDD Loneliness 12 − 2.440 (1.550, 3.838) 0.001 Fewer social activities 67 − 1.408 (0.882, 2.248) 0.290 ANX Loneliness 11 − 1.730 (0.306, 9.786) 0.595 Fewer social activities 45 − 1.706 (0.172, 16.878) 0.720 BIP Loneliness 13 − 1.662 (0.919, 3.004) 0.169 Fewer social activities 60 − 0.573 (0.343, 0.958) 0.096 Note. All statistical tests were two-sided. q-value < 0.05 was considered significant. BMI, body mass index; WHR, waist-hip ratio; WC, waist circumference; HIP, hip circumference; BF%, body fat percentage; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; FG, fasting glucose; FI, fasting insulin; HAb1c, glycated hemoglobin levels; MDD, major depressive disorder; ANX, anxiety disorder; BIP, bipolar disorder; N_SNP, number of SNPS; q-value, P value corrected by False Discovery Rate method. -
[1] Mensah GA, Fuster V, Murray CJL, et al. Global burden of cardiovascular diseases and risks, 1990-2022. J Am Coll Cardiol, 2023; 82, 2350−473. doi: 10.1016/j.jacc.2023.11.007 [2] Powell-Wiley TM, Baumer Y, Baah FO, et al. Social determinants of cardiovascular disease. Circ Res, 2022; 130, 782−99. doi: 10.1161/CIRCRESAHA.121.319811 [3] Cacioppo S, Grippo AJ, London S, et al. Loneliness: clinical import and interventions. Perspect Psychol Sci, 2015; 10, 238−49. doi: 10.1177/1745691615570616 [4] Escalante E, Golden RL, Mason DJ. Social isolation and loneliness: imperatives for health care in a post-COVID World. JAMA, 2021; 325, 520−1. [5] Valtorta NK, Kanaan M, Gilbody S, et al. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart, 2016; 102, 1009−16. [6] Golaszewski NM, LaCroix AZ, Godino JG, et al. Evaluation of social isolation, loneliness, and cardiovascular disease among older women in the US. JAMA Netw Open, 2022; 5, e2146461. doi: 10.1001/jamanetworkopen.2021.46461 [7] Hakulinen C, Pulkki-Råback L, Virtanen M, et al. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK Biobank cohort study of 479 054 men and women. Heart, 2018; 104, 1536−42. doi: 10.1136/heartjnl-2017-312663 [8] Smith RW, Barnes I, Green J, et al. Social isolation and risk of heart disease and stroke: analysis of two large UK prospective studies. Lancet Public Health, 2021; 6, e232−9. [9] Manemann SM, Chamberlain AM, Roger VL, et al. Perceived social isolation and outcomes in patients with heart failure. J Am Heart Assoc, 2018; 7, e008069. doi: 10.1161/JAHA.117.008069 [10] Freak-Poli R, Ikram MA, Franco OH, et al. Depressive symptoms prior to and after incident cardiovascular disease and long-term survival. A population-based study of older persons. Depress Anxiety, 2018; 35, 18−31. doi: 10.1002/da.22689 [11] Philip KE, Bu FF, Polkey MI, et al. Relationship of smoking with current and future social isolation and loneliness: 12-year follow-up of older adults in England. Lancet Reg Health Eur, 2022; 14, 100302. doi: 10.1016/j.lanepe.2021.100302 [12] Henriksen RE, Nilsen RM, Strandberg RB. Loneliness as a risk factor for metabolic syndrome: results from the HUNT study. J Epidemiol Community Health, 2019; 73, 941−6. [13] Lawlor DA, Harbord RM, Sterne JAC, et al. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med, 2008; 27, 1133−63. doi: 10.1002/sim.3034 [14] Burgess S, Daniel RM, Butterworth AS, et al. Network Mendelian randomization: using genetic variants as instrumental variables to investigate mediation in causal pathways. Int J Epidemiol, 2015; 44, 484−95. doi: 10.1093/ije/dyu176 [15] Skrivankova VW, Richmond RC, Woolf BAR, et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomization: the STROBE-MR statement. JAMA, 2021; 326, 1614−21. doi: 10.1001/jama.2021.18236 [16] Day FR, Ong KK, Perry JRB. Elucidating the genetic basis of social interaction and isolation. Nat Commun, 2018; 9, 2457. doi: 10.1038/s41467-018-04930-1 [17] Sudlow C, Gallacher J, Allen N, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med, 2015; 12, e1001779. [18] Song YJ, Zhu C, Shi BQ, et al. Social isolation, loneliness, and incident type 2 diabetes mellitus: results from two large prospective cohorts in Europe and East Asia and Mendelian randomization. eClinicalMedicine, 2023; 64, 102236. doi: 10.1016/j.eclinm.2023.102236 [19] Locke AE, Kahali B, Berndt SI, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature, 2015; 518, 197−206. doi: 10.1038/nature14177 [20] Shungin D, Winkler TW, Croteau-Chonka DC, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature, 2015; 518, 187−96. doi: 10.1038/nature14132 [21] Lu YC, Day FR, Gustafsson S, et al. New loci for body fat percentage reveal link between adiposity and cardiometabolic disease risk. Nat Commun, 2016; 7, 10495. [22] Graham SE, Clarke SL, Wu KHH, et al. The power of genetic diversity in genome-wide association studies of lipids. Nature, 2021; 600, 675−9. doi: 10.1038/s41586-021-04064-3 [23] Chen J, Spracklen CN, Marenne G, et al. The trans-ancestral genomic architecture of glycemic traits. Nat Genet, 2021; 53, 840−60. doi: 10.1038/s41588-021-00852-9 [24] Liu MZ, Jiang Y, Wedow R, et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat Genet, 2019; 51, 237−44. [25] Wray NR, Ripke S, Mattheisen M, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet, 2018; 50, 668−81. doi: 10.1038/s41588-018-0090-3 [26] Forstner AJ, Awasthi S, Wolf C, et al. Genome-wide association study of panic disorder reveals genetic overlap with neuroticism and depression. Mol Psychiatry, 2021; 26, 4179−90. doi: 10.1038/s41380-019-0590-2 [27] Mullins N, Forstner AJ, O'Connell KS, et al. Genome-wide association study of more than 40, 000 bipolar disorder cases provides new insights into the underlying biology. Nat Genet, 2021; 53, 817−29. doi: 10.1038/s41588-021-00857-4 [28] The CARDIoGRAMplusC4D Consortium. A comprehensive 1000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat Genet, 2015; 47, 1121−30. [29] Shen LX, Yang YX, Kuo K, et al. Social isolation, social interaction, and Alzheimer's disease: a mendelian randomization study. J Alzheimers Dis, 2021; 80, 665−72. doi: 10.3233/JAD-201442 [30] Hemani G, Zheng J, Elsworth B, et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife, 2018; 7, e34408. doi: 10.7554/eLife.34408 [31] Emdin CA, Khera AV, Kathiresan S. Mendelian randomization. JAMA, 2017; 318, 1925−6. doi: 10.1001/jama.2017.17219 [32] Burgess S, Scott RA, Timpson NJ, et al. Using published data in Mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol, 2015; 30, 543−52. doi: 10.1007/s10654-015-0011-z [33] Burgess S, Dudbridge F, Thompson SG. Combining information on multiple instrumental variables in Mendelian randomization: comparison of allele score and summarized data methods. Stat Med, 2016; 35, 1880−906. doi: 10.1002/sim.6835 [34] VanderWeele TJ. Mediation analysis: a practitioner's guide. Annu Rev Public Health, 2016; 37, 17−32. [35] MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol, 2007; 58, 593−614. [36] Bowden J, Davey Smith G, Haycock PC, et al. Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol, 2016; 40, 304−14. doi: 10.1002/gepi.21965 [37] Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol, 2015; 44, 512−25. doi: 10.1093/ije/dyv080 [38] Verbanck M, Chen CY, Neale B, et al. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet, 2018; 50, 693−8. doi: 10.1038/s41588-018-0099-7 [39] Zheng J, Baird D, Borges MC, et al. Recent developments in mendelian randomization studies. Curr Epidemiol Rep, 2017; 4, 330−45. [40] Freak-Poli R, Phyo AZZ, Hu J, et al. Are social isolation, lack of social support or loneliness risk factors for cardiovascular disease in Australia and New Zealand? A systematic review and meta-analysis. Health Promot J Austr, 2022; 33 Suppl 1, 278-315. [41] Freak-Poli R, Ryan J, Neumann JT, et al. Social isolation, social support and loneliness as predictors of cardiovascular disease incidence and mortality. BMC Geriatr, 2021; 21, 711. doi: 10.1186/s12877-021-02602-2 [42] Xia N, Li HG. Loneliness, social isolation, and cardiovascular health. Antioxid Redox Signal, 2018; 28, 837−51. doi: 10.1089/ars.2017.7312 [43] Hackett RA, Hamer M, Endrighi R, et al. Loneliness and stress-related inflammatory and neuroendocrine responses in older men and women. Psychoneuroendocrinology, 2012; 37, 1801−9. doi: 10.1016/j.psyneuen.2012.03.016 [44] Jaremka LM, Fagundes CP, Peng J, et al. Loneliness promotes inflammation during acute stress. Psychol Sci, 2013; 24, 1089−97. [45] Tuomisto K, Jousilahti P, Sundvall J, et al. C-reactive protein, interleukin-6 and tumor necrosis factor alpha as predictors of incident coronary and cardiovascular events and total mortality. A population-based, prospective study. Thromb Haemost, 2006; 95, 511−8. doi: 10.1160/TH05-08-0571 [46] Brown EG, Gallagher S, Creaven AM. Loneliness and acute stress reactivity: a systematic review of psychophysiological studies. Psychophysiology, 2018; 55, e13031. doi: 10.1111/psyp.13031 [47] Kilpi F, Konttinen H, Silventoinen K, et al. Living arrangements as determinants of myocardial infarction incidence and survival: a prospective register study of over 300, 000 Finnish men and women. Soc Sci Med, 2015; 133, 93−100. doi: 10.1016/j.socscimed.2015.03.054 [48] Chida Y, Steptoe A, Powell LH. Religiosity/spirituality and mortality. A systematic quantitative review. Psychother Psychosom, 2009; 78, 81−90. [49] Floud S, Balkwill A, Canoy D, et al. Social participation and coronary heart disease risk in a large prospective study of UK women. Eur J Prev Cardiol, 2016; 23, 995−1002. doi: 10.1177/2047487315607056 [50] Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA, 1995; 273, 402−7. doi: 10.1001/jama.1995.03520290054029 [51] Rafiei S, Raoofi S, Baghaei A, et al. Depression prevalence in cardiovascular disease: global systematic review and meta-analysis. BMJ Support Palliat Care, 2023; 13, 281−9. doi: 10.1136/spcare-2022-003884 [52] Heinberg LJ, Steffen K. Social isolation and loneliness during the COVID-19 pandemic: impact on weight. Curr Obes Rep, 2021; 10, 365−70. [53] Cacioppo JT, Cacioppo S, Capitanio JP, et al. The neuroendocrinology of social isolation. Annu Rev Psychol, 2015; 66, 733−67. doi: 10.1146/annurev-psych-010814-015240 [54] Steptoe A, Brydon L. Associations between acute lipid stress responses and fasting lipid levels 3 years later. Health Psychol, 2005; 24, 601−7. [55] Wootton RE, Greenstone HSR, Abdellaoui A, et al. Bidirectional effects between loneliness, smoking and alcohol use: evidence from a Mendelian randomization study. Addiction, 2021; 116, 400−6. doi: 10.1111/add.15142 [56] De Hert M, Detraux J, Vancampfort D. The intriguing relationship between coronary heart disease and mental disorders. Dialogues Clin Neurosci, 2018; 20, 31−40. doi: 10.31887/DCNS.2018.20.1/mdehert [57] Siegrist J, Sies H. Disturbed redox homeostasis in oxidative distress: a molecular link from chronic psychosocial work stress to coronary heart disease? Circ Res, 2017; 121, 103-5. [58] Li HG, Xia N. The role of oxidative stress in cardiovascular disease caused by social isolation and loneliness. Redox Biol, 2020; 37, 101585. doi: 10.1016/j.redox.2020.101585 [59] Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; american heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation, 2009; 120, 1640−5. doi: 10.1161/CIRCULATIONAHA.109.192644 [60] Kopin L, Lowenstein CJ. Dyslipidemia. Ann Intern Med, 2017; 167, ITC81−96. doi: 10.7326/AITC201712050 [61] Zhu ZW, Wang K, Hao XJ, et al. Causal graph among serum lipids and glycemic traits: a mendelian randomization study. Diabetes, 2022; 71, 1818−26. [62] Guignard R, Quatremère G, Pasquereau A, et al. Barriers against and motivations for quitting smoking during the COVID-19 health crisis: results of a qualitative study in france. Int J Environ Res Public Health, 2022; 19, 13051. doi: 10.3390/ijerph192013051 [63] Warmbrunn MV, Boulund U, Aron-Wisnewsky J, et al. Networks of gut bacteria relate to cardiovascular disease in a multi-ethnic population: the HELIUS study. Cardiovasc Res, 2024; 120, 372−84. doi: 10.1093/cvr/cvae018 [64] Lecour S, Du Pré BC, Bøtker HE, et al. Circadian rhythms in ischaemic heart disease: key aspects for preclinical and translational research: position paper of the ESC working group on cellular biology of the heart. Cardiovasc Res, 2022; 118, 2566−81. doi: 10.1093/cvr/cvab293 [65] Krittayaphong R. Cardiovascular risk prediction model in asians: current status and future direction. JACC Asia, 2024; 4, 275−8. [66] Yang XL, Li JX, Hu DS, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-PAR project (prediction for ASCVD risk in China). Circulation, 2016; 134, 1430−40. doi: 10.1161/CIRCULATIONAHA.116.022367 [67] Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet, 2014; 23, R89−98. doi: 10.1093/hmg/ddu328 -
 24298+Supplementary Materials.pdf
24298+Supplementary Materials.pdf

-




 下载:
下载:





 Quick Links
Quick Links