-
It is essential to use evidence-based and cost-effective drugs in the management of patients with cardiovascular diseases (CVDs), because the task of secondary prevention is arduous given the burden of disease and sparse healthcare resources in China[1]. However, China is the only country in the world where Western medicine and traditional Chinese medicine (TCM) are practiced alongside each other at every level of the healthcare system. There are several TCM products (or Zhong Cheng Yao) for CVDs in China, which are active ingredients or compounds extracted from herbs. Currently, more than 90% of the urban and rural Chinese population have sought for TCM in their lifetimes[2]. In this study, we aimed to investigate the usage and regional variation of well-established secondary prevention drugs [antiplatelet drugs, β-blockers, angiotensin-converting-enzyme inhibitor/angiotensin receptor blockers (ACEI/ARBs), and statins] and TCM products at the community level using data from the global Prospective Urban and Rural Epidemiological (PURE) study in China.
-
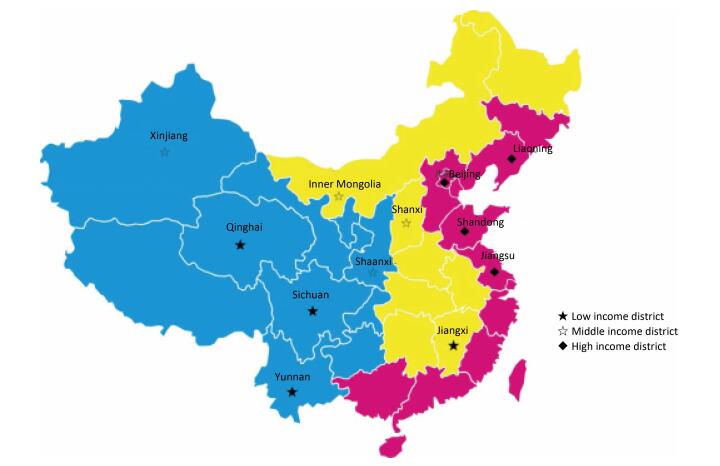
The methods of the PURE study have been described elsewhere[3]. All individuals within the eligible households and who provided written informed consent were enrolled and evaluated between May 2005 and December 2009. In the PURE-China study, to reflect the variation in economic development and geographical diversity in China, we selected the sampled population according to the following geographic areas: The Eastern, Central, and Western areas (Supplementary Figure 1 available in www.besjournal.com). Eastern China is along the sea coast and is the most developed area, while Western China is the least developed area. This study was approved by the Ethics Committee of the Cardiovascular Institute and Fu Wai Hospital, Chinese Academy of Medical Sciences, and Peking Union Medical College.
-
In this study, CVDs patients were defined as those who either had CHD or stroke, and this was assessed using standardized questionnaires. CHD was evaluated on the basis of self-reported angina, myocardial infarction, coronary artery bypass graft surgery, or percutaneous coronary intervention. Stroke was ascertained based on self-reports. Use of antiplatelet drugs, β-blockers, ACEI/ARBs, statins, diuretics, and TCM products was analyzed. The quality of data collection was maintained via standardized protocols and centralized training.
-
We compared the difference between urban and rural areas using the analysis of variance for continuous variables and the χ2 statistic for categorical variables. We adjusted proportions for individual-level factors with a generalized linear model as appropriate and used the Cochran-Armitage test to assess trends in the subgroups. Separate regression analyses were carried out for each region (urban-rural areas, Eastern, Central, and Western China). All analyses were performed using SAS 9.1.3 (SAS, Cary, NC).
In 46, 285 individuals who provided complete measurements and questionnaires, 2, 407 (5.2%) had CHD and 872 (1.5%) had stroke. Compared with individuals with CVDs in urban communities, those in rural communities tended to be younger, more likely to be women or have a lower education level, but were less likely to have a higher body mass index (BMI) or diabetes (Supplementary Table 1 available in www.besjournal.com).
Table Supplement Table 1. Baseline Characteristics
Item CHD Stroke CHD or Stroke Urban Rural P Urban Rural P Urban Rural P N 1, 431 976 542 330 1, 841 1, 229 Age (y) 59.5±7.7 55.5+ 9.3 < 0.0001 60.0 ±7.8 56.9 ± 8.4 < 0.0001 59.4 ± 7.8 55.8 ±9.1 < 0.0001 Sex (female) 886 (61.9%) 666 (68.2%) 0.0015 266 (49.1%) 167 (50.6%) 0.6615 1078 (58.6%) 782 (63.6%) 0.0048 Education < 0.0001 < 0.0001 < 0.0001 None, primary school or unknown 364 (25.4%) 696 (71.3%) 160 (29.5%) 200 (60.6%) 484 (26.3%) 851 (69.2%) Secondary or high school 683 (47.7%) 260 (26.6%) 265 (48.9%) 123 (37.3%) 886(48.1%) 354 (28.8%) Trade, college, or university 384 (26.8%) 20 (2.1%) 117(21.6%) 7 (2.1%) 471 {25.6%) 24 (2.0%) Body mass index (kg/m2) < 0.0001 < 0.0001 < 0.0001 < 24 443 (31.0%) 414(43.1%) 174 (32.3%) 149 (46.7%) 576 (31.4%) 528 (43.9%) 24-28 612 (43.0%) 343 (35.8%) 235 (43.6%) 116(36.4%) 795 (43.4%) 429 (35.7%) ≥28 370 (26.0%) 202 (21.1%) 130(24.1%) 54 (16.9%) 462 (25.2%) 245 (20.4%) Diabetes 228 (16.0%) 83 (8.6%) < 0.0001 102 (18.8%) 46 (13.9%) 0.0626 285(15.5%) 108 (8.8%) < 0.0001 Smoking 0.0008 0.3569 0.0007 Non-smoker 1047 (73.2%) 765 (78.4%) 348 (64.2%) 226 (68.5%) 1295 (70.3%) 932 (75.8%) Former smoker 165 (11.5%) 69 (7.1%) 82 (15.1%) 40 (12.1%) 226(12.3%) 103 (8.4%) Current smoker 219 (15.3%) 142(14.6%) 112 (20.7%) 64 (19.4%) 320(17.4%) 194 (15.8%) Years since diagnosis 5.0 (3.0-10.0) 4.0(2.0-8.01 < 0.0001 4.0 (2.0-7.0) 4.0(2.0-7.0) 0.1787 5.0 (2.0-10.0) 4.0 (2.0-8.0) < .0001 Note. Data are n (%) or mean (SD). Nearly 80% individuals with CHD and 73% individuals with stroke were not taking any proven secondary prevention drug (antiplatelet drugs, β-blockers, ACEI/ARBs, and statins), with a higher rate in rural than in urban areas (CHD 85.9% vs. 75.4%, P < 0.0001; stroke 78.2% vs. 69.9%, P < 0.0001). The use of ACEI/ARBs, β-blockers, and statins was all less than 10%, in both urban and in rural areas. Only 5 (0.4%) individuals were taking statins in the rural areas. As shown in Table 1, 32.9% of participants with CVDs were taking TCM products, much higher than the use of antiplatelet drugs (19.1%), ACEI/ARBs (8.6%), β-blockers (6.2%), and statins (1.7%). Similar proportions of participants with CHD or stroke in the urban and rural areas were taking TCM products.
Table 1. Rate of Drug Use in Participants with CVDs by Rural/urban Region
Items Total Urban Rural Ptrend CVDs n = 3, 070 n = 1, 841 n = 1, 229 ACEI/ARBs (%) 264 (8.6) 173(9.4) 91 (7.4) 0.0537 CCBs (%) 457 (14.9) 348 (18.9) 109 (8.9) < 0.0001 β-blockers (%) 190 (6.2) 160 (8.7) 30 (2.4) < 0.0001 Diuretics 69 (2.2) 58 (3.2) 11 (0.9) < 0.0001 Antiplatelet drugs (%) 585 (19.1) 356 (19.3) 229 (18.6) 0.6264 Statins (%) 53 (1.7) 48 (2.6) 5 (0.4) < 0.0001 Blood-pressure-lowering drugs (%) 1, 142 (37.2) 797 (43.3) 345 (28.1) < 0.0001 TCM products (%) 1, 010 (32.9) 601 (32.7) 409 (33.3) 0.7142 Coronary heart disease n = 2, 407 n = 1, 431 n = 976 ACEI/ARBs (%) 187 (7.8) 124 (8.7) 63 (6.5) 0.0467 CCBs (%) 316 (13.1) 245 (17.1) 71 (7.3) < 0.0001 β-blockers (%) 163 (6.8) 135 (9.4) 28 (2.9) < 0.0001 Diuretics (%) 51 (2.1) 41 (2.9) 10 (1.0) 0.0021 Antiplatelet drugs (%) 386 (16.0) 240 (16.8) 146 (15.0) 0.2341 Statins (%) 49 (2.0) 45 (3.1) 4 (0.4) < 0.0001 Blood-pressure-lowering drugs (%) 843 (35.0) 593 (41.4) 250 (25.6) < 0.0001 TCM products (%) 773 (32.1) 466 (32.6) 307 (31.5) 0.5670 Stroke n = 872 n = 542 n = 330 ACEI/ARBs (%) 101 (11.6) 64 (11.8) 37 (11.2) 0.7897 CCBs (%) 190 (21.8) 144 (26.6) 46 (13.9) < 0.0001 β-blockers (%) 36 (4.1) 34 (6.3) 2 (0.6) < 0.0001 Diuretics (%) 28 (3.2) 25 (4.6) 3 (0.9) 0.0023 Antiplatelet drugs (%) 258 (29.6) 155 (28.6) 103 (31.2) 0.4120 Statins (%) 7 (0.8) 6 (1.1) 1 (0.3) 0.1969 Blood-pressure-lowering drugs (%) 404 (46.3) 280 (51.7) 124 (37.6) < 0.0001 TCM products (%) 312 (35.8) 180 (33.2) 132 (40.0) 0.0425 Note. ACEI = angiotensin-converting enzyme inhibitors. ARBs = angiotensin II receptor blockers. CCBs = calcium channel blockers. CVDs = cardiovascular diseases. TCM = traditional Chinese medicine. Fewer people in the CHD group compared to the stroke group took blood pressure-lowering drugs (35.0% vs. 46.3%; P < 0.0001). Compared with participants with stroke, those with CHD were less likely to take antiplatelet drugs (CHD 16.0% vs. stroke 29.6%; P < 0.0001), but were more likely to take β-blockers (CHD 6.8% vs. stroke 4.1%; P = 0.0051) and statins (CHD 2.0% vs. stroke 0.8%; P = 0.0161).
The elderly were more likely than the younger to take effective secondary prevention drugs; 22.3% of the patients aged 60 years or older took antiplatelet drugs, compared with 19.2% of those aged 50-60 years and 10.5% of those aged less than 50 years. Patients with higher educational levels and household income tended to use effective drugs more often compared to those with lower educational levels and household income. Older persons took TCM products more often than effective secondary prevention drugs (Supplementary Figure 2 available in www.besjournal.com).
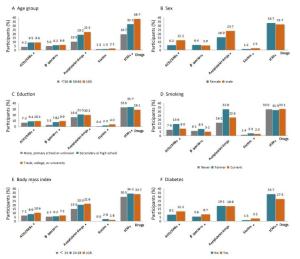
Figure Supplement Figure 2. Drug use in par cipants with CVDs Classified by age (A), sex (B), educa on (C), smoking history (D), bodymass index (E), and diabetes status (F). ACEI = angiotensin-conver ng enzyme inhibitor; ARB=angiotensin-receptor blocker; TCM = tradi onal Chinese medicine; *P < 0.05.
Those in Western China had the lowest rates of secondary prevention drugs use (Table 2), where only 5.3%, 4.3%, 5.3%, and 0.5% of patients were taking antiplatelet drugs, β-blockers, ACEI/ARBs, and statins, respectively. TCM products usage also differed greatly between the three parts of China. More than 40% of patients in Central China were taking TCM products, higher than those in Eastern (37.3%) and Western China (16.6%).
Table 2. Rate of Drug use in Participants with CVDs by Eastern/Central/Western China
Items Eastern
(n = 1663)Central
(n = 635)Western
(n = 772)P ACEI/ARBs (%) 173 (10.4) 50 (7.9) 41 (5.3) < 0.0001 CCBs (%) 261 (15.7) 157 (24.7) 39 (5.1) < 0.0001 β-blockers (%) 98 (5.9) 59 (9.3) 33 (4.3) < 0.0001 Diuretics 34 (2.0) 20 (3.2) 15 (1.9) < 0.0001 Antiplatelet drugs (%) 392 (23.6) 152 (23.9) 41 (5.3) < 0.0001 Statins (%) 26 (1.6) 23 (3.6) 4 (0.5) < 0.0001 Blood-pressure-lowering drugs (%) 716 (43.1) 283 (44.6) 143 (18.5) < 0.0001 TCM products (%) 621 (37.3) 261 (41.1) 128 (16.6) < 0.0001 Note. ACEI = angiotensin-converting enzyme inhibitors. ARBs = angiotensin II receptor blockers. CCBs = calcium channel blockers. CVDs = cardiovascular diseases. TCM = traditional Chinese medicine. As shown in Table 3, after adjusting for sex and age, BMI, smoking, household income, diabetes, and educational status, lower rates of secondary prevention treatment (0.41; 95% CI 0.34-0.51) and TCM products use (0.50; 95% CI 0.44-0.56) were evident in Western China compared to the Eastern China. Patients with CVDs in the rural area used less secondary prevention treatment (0.60; 95% CI 0.40-0.78), but more TCM products (1.36; 95% CI 1.23-1.50) than their counterparts in urban areas.
Table 3. Multiple Logistic Regression Analyses of Effective Secondary Prevention Drugs and TCM Products by Eastern/Central/Western China and Rural/Urban
Items Secondary Prevention Drugs P TCM Products P OR (95% CI) OR (95% CI) Areasa Eastern China 1 1 Middle China 0.94 (0.80-1.10) 0.4476 1.28 (1.16-1.41) < 0.0001 Western China 0.41 (0.34-0.51) < 0.0001 0.50 (0.44-0.56) < 0.0001 Locationsb Urban 1 Rural 0.60 (0.40-0.78) < 0.0001 1.36 (1.23-1.50) < 0.0001 Note. TCM = traditional Chinese medicine; OR = odds ratios; CI = confidence interval; aBase line category: Eastern area; bBase line category: rural. To our knowledge, this is an advanced study that has attempted to describe the community-level estimates of not only proven preventive drug use, but also TCM products in CVD patients in China. Our study demonstrated a low rate of effective secondary prevention drug use and a relatively high proportion of TCM products usage in CVD patients, with regional variations reflecting health financing and healthcare utilization.
There are some possible explanations for the insufficient use of effective secondary prevention drugs in Chinese communities. First, patients in communities may lack information and the basic knowledge about the secondary prevention of CVDs[4]. Second, there is a significant gap between practice and guidelines even in large hospitals in China[5]. The percentage of the physicians who were aware of the control targets and prevention measures recommended in the Chinese national guidelines for stroke was generally lower than reported for developed countries[6].Third, it is costly for adults to access medical facilities, especially those in the rural areas. Such costs include travel time to a medical facility, long waiting times in the facility, and financial costs. Moreover, most Chinese individuals are concerned about the possible side effects of statins, especially liver enzyme elevation[7]. In addition, most of the trials have been undertaken in Western populations and there is possibly the belief that Chinese patients may respond differently to these drugs[7].
The high rates of TCM use for secondary prevention may consume valuable healthcare resources. We noted a higher rate of TCM products usage in rural areas compared to urban areas. This is consistent with a study[8] that noted that while the utilization rate of TCM had declined greatly in China, the decline in the use of TCM was much less drastic in rural areas than in urban areas. The preference for TCM may stem from perceptions that TCM is beneficial to health maintenance or tonic care. Contrary to the theory of TCM that emphasizes the self-healing power of man for curing diseases and maintaining fitness, there is the increasing availability and use of commercially produced TCM products in solid form in China. One-third of the medications in the essential drug list, which is designed to make medication more affordable for Chinese citizens, are TCM products[9]. However, TCM products are not recommended in the current national guidelines of stroke and CHD. China should focus on increasing the quality, quantity, and accessibility of clinical evidence to support claims for the effectiveness of TCM products.
Patients with CVDs in rural areas and Western China had a lower rate of both effective secondary prevention drug and TCM products use compared to those in urban areas and Eastern China. To a large extent, disparities in local economic conditions may be responsible for the unequal distribution of health resources. In China, it is the responsibility of local governments to fund majority of government spending for both health provision and health insurance. In less developed regions, the fiscal budget of local governments, usually, is rarely enough to fund health provision. This fact reinforces the regional inequality of healthcare. Investment in health resources leads to differences in the distribution of other aspects of healthcare. It is necessary to improve economic development in less developed regions and to improve health policies and the public health system to address the needs of the general population.
Several limitations exist in the current study. First, the diagnoses of CHD and stroke were self-reported, and therefore, a small proportion of individuals might not have had vascular disease. Second, drug use was self-reported and did not take into account adherence to reported treatments.
However, our study has several strengths; we have provided the only community-level estimates, to date, of proven preventive drug and TCM products usage in individuals with CVDs from urban and rural settings and across Eastern, Central, and Western China. Using prospective data excluded potential biases related to the collection of data only for patients who visit clinics or hospitals; we identified and described the unique patterns of drug use in community citizens. The findings of the substantial underuse and regional variation of effective secondary prevention drugs and the high percentage of TCM products usage in Chinese communities provide some insight into the urgent need for an evidence-based approach to clinical practice in China.
doi: 10.3967/bes2017.059
Regional Variations in Medication Usage for Cardiovascular Diseases at the Community Level in China (PURE-China Study)
-
Abstract: We investigated the usage of secondary prevention drugs and traditional Chinese medicine (TCM) products in individuals with cardiovascular diseases (CVDs) at the community level in China. Among 2, 407 participants with self-reported coronary heart disease (CHD) and 872 with stroke, nearly 80% of individuals with CHD and 73% of individuals with stroke were not taking any proven secondary prevention drug. However, 32.9% of them took TCM products. Patients with CVDs in rural areas used less secondary prevention treatment, but more TCM products than their counterparts in the urban regions. After adjusting for confounding factors, lower rates of secondary prevention treatment were evident in Western China compared with Eastern China, which was more developed. Systematic change is needed to promote the development of evidence-based medicine at the community level in China.
-
Supplement Table 1. Baseline Characteristics
Item CHD Stroke CHD or Stroke Urban Rural P Urban Rural P Urban Rural P N 1, 431 976 542 330 1, 841 1, 229 Age (y) 59.5±7.7 55.5+ 9.3 < 0.0001 60.0 ±7.8 56.9 ± 8.4 < 0.0001 59.4 ± 7.8 55.8 ±9.1 < 0.0001 Sex (female) 886 (61.9%) 666 (68.2%) 0.0015 266 (49.1%) 167 (50.6%) 0.6615 1078 (58.6%) 782 (63.6%) 0.0048 Education < 0.0001 < 0.0001 < 0.0001 None, primary school or unknown 364 (25.4%) 696 (71.3%) 160 (29.5%) 200 (60.6%) 484 (26.3%) 851 (69.2%) Secondary or high school 683 (47.7%) 260 (26.6%) 265 (48.9%) 123 (37.3%) 886(48.1%) 354 (28.8%) Trade, college, or university 384 (26.8%) 20 (2.1%) 117(21.6%) 7 (2.1%) 471 {25.6%) 24 (2.0%) Body mass index (kg/m2) < 0.0001 < 0.0001 < 0.0001 < 24 443 (31.0%) 414(43.1%) 174 (32.3%) 149 (46.7%) 576 (31.4%) 528 (43.9%) 24-28 612 (43.0%) 343 (35.8%) 235 (43.6%) 116(36.4%) 795 (43.4%) 429 (35.7%) ≥28 370 (26.0%) 202 (21.1%) 130(24.1%) 54 (16.9%) 462 (25.2%) 245 (20.4%) Diabetes 228 (16.0%) 83 (8.6%) < 0.0001 102 (18.8%) 46 (13.9%) 0.0626 285(15.5%) 108 (8.8%) < 0.0001 Smoking 0.0008 0.3569 0.0007 Non-smoker 1047 (73.2%) 765 (78.4%) 348 (64.2%) 226 (68.5%) 1295 (70.3%) 932 (75.8%) Former smoker 165 (11.5%) 69 (7.1%) 82 (15.1%) 40 (12.1%) 226(12.3%) 103 (8.4%) Current smoker 219 (15.3%) 142(14.6%) 112 (20.7%) 64 (19.4%) 320(17.4%) 194 (15.8%) Years since diagnosis 5.0 (3.0-10.0) 4.0(2.0-8.01 < 0.0001 4.0 (2.0-7.0) 4.0(2.0-7.0) 0.1787 5.0 (2.0-10.0) 4.0 (2.0-8.0) < .0001 Note. Data are n (%) or mean (SD). Table 1. Rate of Drug Use in Participants with CVDs by Rural/urban Region
Items Total Urban Rural Ptrend CVDs n = 3, 070 n = 1, 841 n = 1, 229 ACEI/ARBs (%) 264 (8.6) 173(9.4) 91 (7.4) 0.0537 CCBs (%) 457 (14.9) 348 (18.9) 109 (8.9) < 0.0001 β-blockers (%) 190 (6.2) 160 (8.7) 30 (2.4) < 0.0001 Diuretics 69 (2.2) 58 (3.2) 11 (0.9) < 0.0001 Antiplatelet drugs (%) 585 (19.1) 356 (19.3) 229 (18.6) 0.6264 Statins (%) 53 (1.7) 48 (2.6) 5 (0.4) < 0.0001 Blood-pressure-lowering drugs (%) 1, 142 (37.2) 797 (43.3) 345 (28.1) < 0.0001 TCM products (%) 1, 010 (32.9) 601 (32.7) 409 (33.3) 0.7142 Coronary heart disease n = 2, 407 n = 1, 431 n = 976 ACEI/ARBs (%) 187 (7.8) 124 (8.7) 63 (6.5) 0.0467 CCBs (%) 316 (13.1) 245 (17.1) 71 (7.3) < 0.0001 β-blockers (%) 163 (6.8) 135 (9.4) 28 (2.9) < 0.0001 Diuretics (%) 51 (2.1) 41 (2.9) 10 (1.0) 0.0021 Antiplatelet drugs (%) 386 (16.0) 240 (16.8) 146 (15.0) 0.2341 Statins (%) 49 (2.0) 45 (3.1) 4 (0.4) < 0.0001 Blood-pressure-lowering drugs (%) 843 (35.0) 593 (41.4) 250 (25.6) < 0.0001 TCM products (%) 773 (32.1) 466 (32.6) 307 (31.5) 0.5670 Stroke n = 872 n = 542 n = 330 ACEI/ARBs (%) 101 (11.6) 64 (11.8) 37 (11.2) 0.7897 CCBs (%) 190 (21.8) 144 (26.6) 46 (13.9) < 0.0001 β-blockers (%) 36 (4.1) 34 (6.3) 2 (0.6) < 0.0001 Diuretics (%) 28 (3.2) 25 (4.6) 3 (0.9) 0.0023 Antiplatelet drugs (%) 258 (29.6) 155 (28.6) 103 (31.2) 0.4120 Statins (%) 7 (0.8) 6 (1.1) 1 (0.3) 0.1969 Blood-pressure-lowering drugs (%) 404 (46.3) 280 (51.7) 124 (37.6) < 0.0001 TCM products (%) 312 (35.8) 180 (33.2) 132 (40.0) 0.0425 Note. ACEI = angiotensin-converting enzyme inhibitors. ARBs = angiotensin II receptor blockers. CCBs = calcium channel blockers. CVDs = cardiovascular diseases. TCM = traditional Chinese medicine. Table 2. Rate of Drug use in Participants with CVDs by Eastern/Central/Western China
Items Eastern
(n = 1663)Central
(n = 635)Western
(n = 772)P ACEI/ARBs (%) 173 (10.4) 50 (7.9) 41 (5.3) < 0.0001 CCBs (%) 261 (15.7) 157 (24.7) 39 (5.1) < 0.0001 β-blockers (%) 98 (5.9) 59 (9.3) 33 (4.3) < 0.0001 Diuretics 34 (2.0) 20 (3.2) 15 (1.9) < 0.0001 Antiplatelet drugs (%) 392 (23.6) 152 (23.9) 41 (5.3) < 0.0001 Statins (%) 26 (1.6) 23 (3.6) 4 (0.5) < 0.0001 Blood-pressure-lowering drugs (%) 716 (43.1) 283 (44.6) 143 (18.5) < 0.0001 TCM products (%) 621 (37.3) 261 (41.1) 128 (16.6) < 0.0001 Note. ACEI = angiotensin-converting enzyme inhibitors. ARBs = angiotensin II receptor blockers. CCBs = calcium channel blockers. CVDs = cardiovascular diseases. TCM = traditional Chinese medicine. Table 3. Multiple Logistic Regression Analyses of Effective Secondary Prevention Drugs and TCM Products by Eastern/Central/Western China and Rural/Urban
Items Secondary Prevention Drugs P TCM Products P OR (95% CI) OR (95% CI) Areasa Eastern China 1 1 Middle China 0.94 (0.80-1.10) 0.4476 1.28 (1.16-1.41) < 0.0001 Western China 0.41 (0.34-0.51) < 0.0001 0.50 (0.44-0.56) < 0.0001 Locationsb Urban 1 Rural 0.60 (0.40-0.78) < 0.0001 1.36 (1.23-1.50) < 0.0001 Note. TCM = traditional Chinese medicine; OR = odds ratios; CI = confidence interval; aBase line category: Eastern area; bBase line category: rural. -
[1] Hu SS, Kong LZ, Gao RL, et al. Outline of the report on cardiovascular disease in China, 2010. Biomed Environ Sci, 2012, 25:251-6. http://www.besjournal.com/Articles/Archive/archive/No3/201207/P020120712460143315034.pdf [2] Xu J, Yang Y. Traditional Chinese medicine in the Chinese health care system. Health Policy, 2009, 90:133-9. doi: 10.1016/j.healthpol.2008.09.003 [3] Li W, Gu H, Teo KK, et al. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47, 000 people from china. J Hypertens, 2016, 34:39-46. doi: 10.1097/HJH.0000000000000745 [4] Wei JW, Wang JG, Huang Y, et al. Secondary prevention of ischemic stroke in urban China. Stroke, 2010, 41:967-74. doi: 10.1161/STROKEAHA.109.571463 [5] Angina treatment pattern survey collaborative group. Current status of medical therapy of chronic stable angina pectoris in mainland of China: The second survey. Zhonghua Xin Xue Guan Bing Za Hhi, 2010, 38:1060-4. (In Chinaese) https://www.researchgate.net/publication/296850911_Current_status_of_medical_therapy_of_chronic_stable_angina_pectoris_in_mainland_of_China_the_second_survey [6] Wu J, Jia LF, Jia JP. Awareness of secondary stroke prevention guidelines among neurologists in china: A cross-sectional online survey. Chin Med J (Engl), 2012, 125:1867-70. http://industry.wanfangdata.com.cn/dl/Detail/Periodical?id=Periodical_zhcmj201211005 [7] Liao JK. Safety and efficacy of statins in Asians. Am J Cardiol, 2007, 99:410-4. doi: 10.1016/j.amjcard.2006.08.051 [8] Jin L. From mainstream to marginal? Trends in the use of Chinese medicine in china from 1991 to 2004. Soc Sci Med, 2010, 71:1063-7. doi: 10.1016/j.socscimed.2010.06.019 [9] Guan X, Liang H, Xue Y, et al. An analysis of China's national essential medicines policy. J Public Health Policy, 2011, 32:305-19. doi: 10.1057/jphp.2011.34 -





 下载:
下载:



 Quick Links
Quick Links